Multicomponent Interventions to Increase Breast Cancer Screening
| Author & Year | Intervention Setting, Description, and Comparison Group(s) | Study Population Description and Sample Size | Effect Measure (Variables) | Results, including Test Statistics and Significance | Follow-up Time |
| Mohtasham Ghaffari et. al 2018 | This study was based in Karaj City, Iran Cluster sampling was used to enroll participants from two urban health care centers, which were randomly split into an experimental group where participants attended two 50 minute educational sessions, and a control group. The integrated behavioral model was used. | 138 women above 35 years of age were enrolled from Karaj City attending two health centers in Mohammad Shahr City with the same social, economic and cultural conditions | Age, social, economic, cultural status, demography | No statistically significant differences were found between the experimental and control group demographic variables based on chi square analysis There were statistically significant differences in knowledge structure, perceived susceptibility, perceived severity, perceived benefits and perceived barriers, self-efficacy and perceived barriers for mammography, BSE and subjective norms after training compared with the control group. Behavioral intention, BSE behavioral intention and mammography behavioral intention also showed a statistically significant result following intervention. However, mammography behavior did not. This study concluded that there is a benefit to implementing an educational intervention to promote breast cancer screening among the population studied | Questionnaires were given before the intervention, immediately after, and 2 months following the intervention |
| Dunn, S.F. et al. 2017 | Cancer Awareness: Ready for Education and Screening (CARES) was conducted in Toronto, Canada to improve breast and cervical screening among marginalized women. Based on provincial data collected from 1998-2014, participants were matched to up to 3 controls based on age, geography and pre-education screening status. | 1993 women from around Toronto, Canada, participated in 145 educational sessions provided in 20 languages; 419 women were matched with controls based on age, geography, pre-education screening status | Age, geography, pre-education screening status, | Among UNS CARES participants: 26% had Pap conducted, and 36% received a mammogram vs. 9% and 14% in the control group. ORs for screening within 8 months of follow-up among UNS CARES participants: 5.1 (2.4, 10.9 CI) for Pap and 4.2 (2.3, 7.8 CI) for mammography | 8 months |
| Elder, J.P. et al, 2017 | A randomized controlled trial was conducted with 436 women attending 16 Catholic churches who were split into a cancer screening group or physical activity intervention group.Those in the cancer screening intervention group received educational information about cancer screening through Promotoras. They also received up to two motivational interviewing calls over the course of the 1-year intervention from the Promotoras and Promotoras were allowed to accompany the participants to screening appointments if desired. Churches also offered cancer screening classes | 436 adult Latina women attending 16 Catholic churches in San Diego County between the ages of 18-65 | Age, church attendance, proximity to the church, education, household income, employment status, country of birth, years living in the US, health insurance status, health conditions, cancer knowledge | Breast cancer screening rates improved from 44% to 61% for mammograms, and 47-63% for breast exams in the 12-month follow-up assessment in the cancer screening group. This group also showed a decrease in scores for perceived barriers to breast cancer | 12 months follow-up following baseline and 24 month post baseline |
Based on the evidence found in recent studies, using a multicomponent intervention approach to helping increase breast cancer screening amongst women, is strongly recommended. Based on research conducted by the Community Guide, multicomponent interventions which may consist of educational components, client reminders, better delivery of screening services, and reduced economic or structural barriers, have proven to be effective in increasing screening rates among women who may not have previously received these services. These findings were supported by the resources summarized above.
No changes were made to the recommendations to use a multicomponent approach in order to increase breast cancer screening. Educational strategies where women participated in courses appeared to increase the likelihood of women voluntarily receiving mammograms. (Elder et. al, 2017 & Mohtashem et. al, 2018) The information is often offered in multiple languages in order for it to be accessible by women of different backgrounds. In addition, reminders such as a letter or verbal communication about the benefits of breast screening from a health professional also proved effective in encouraging women to receive mammograms. Although the Community Guide suggests that there is limited information about the efficacy of interventions that provide language translation services, based on Dunn’s study from 2017, I would categorize this strategy as “recommended”, although this may vary based on geographic location. There is still limited information on intervention costs in comparison with intervention benefits.
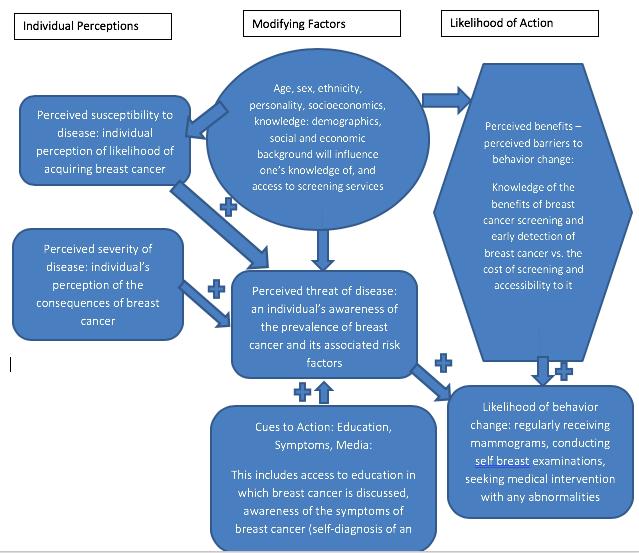
Part II. Theoretical Framework/Model
- Briefly describe in text the theory you selected, including each of the constructs, and why. You may reference evidence from your table above or other sources. (20 points)
The Health Belief Model acts on the principle that people may change a behavior given that the perceived benefits of the behavioral change outweighs the perceived barriers associated with the change. This decision is also likely influenced by the consequences (threat) of not undergoing the behavior change. The Health Belief Model has been used in prevention of illness and can be used to predict breast cancer screening behaviors. (Jones et. al, 2015) The constructs that make up this model include perceived susceptibility, perceived severity of disease, perceived threat of disease, perceived benefits of the intervention, perceived barriers to the intervention, cues to action, age, sex, socioeconomics, knowledge, ethnicity, and personality. (Darvishpour et. al 2018)
Perceived susceptibility: This refers to a person’s personal belief that they will get a disease. Specific to breast cancer, a woman is more likely to pursue breast cancer screening if her perception of the likelihood of getting breast cancer based on her demographic characteristics, is higher.
Perceived threat to disease: This refers to the awareness that one has of the consequences of a disease. If we consider breast cancer specifically, a woman who is aware of the prevalence of breast cancer amongst women and the increased likelihood of its occurrence with age is more likely to pursue breast cancer screening.
Cues to Action: These consist of education, symptoms, and media. Cues to Action influence one’s perceived threat to disease. For example, if a woman is educated about the dangers and prevalence of breast cancer and the need to diagnose it early in order to treat it, then she is more likely to pursue breast cancer screening.
Age, sex, ethnicity, personality, socioeconomics, knowledge: These are modifying factors that influence the perceived susceptibility to disease, perceived severity to disease and perceived benefits or barriers of intervention.
Perceived benefits: The perceived benefits of an intervention strategy, when compared to an individual’s perceived barriers, will determine the likelihood of behavior change. Someone who perceives the benefits of breast cancer screening to outweigh the barriers associated with it, will be more likely to pursue it.
- Draw a diagram to illustrate your conceptual model, making sure to include an indication of the hypothesized direction of the relation (positive or inverse) between the constructs. You may use plus or minus signs, up and down arrows, or another method as long as it is clear. Do not create a logic model. (16 points)
Part III. Logic Model, Causal and Intervention Hypotheses, and Intervention Strategies
- Brieflydescribe the target population and program setting for your intervention. Think about the course materials and discussion of health disparities. Provide evidence for why your target population is a health disparate group. This can include, but is not limited to, description of greater risk or prevalence of disease or risk factors, being in a minority group or low-resource geographic area. Provide citations as appropriate. (5 points)
The target population for my proposed intervention is women of minority backgrounds in Clarkston, Georgia. A majority of the population in Clarkston City is foreign-born, of refugee backgrounds, making health care harder to acquire, especially when taking into consideration social or cultural influences such as language barriers. This area is also of a lower-resource and lower socio-economic status. Clarkston has a population of 12,757 people of which 49.8% are female. 52.9% of the population is foreign born. 33.2% of the population does not have health insurance. 33% of the population is living in poverty. 66.5% of the population above the age of 25 has received high-school level education, and 21.6% of this demographic has a Bachelor’s degree or higher. (US Census Bureau)
- Explicitly state the Intervention Methods for the program (minimum of 3), the theory from which they are derived if different from your theoretical model in items 4 and 5, and a brief description of how they align with that theory. Use the Table template below. (18 points)
- Explicitly describe the Intervention Strategies for each Intervention Method (should have at least one strategy per method). Enter this information into the table below. (9 points)
| Intervention Method | Alignment with Theory | Intervention Strategy |
| Increasing knowledge about breast cancer screening/diagnosis/treatment amongst women in Clarkston City (18+) | Providing educational support about breast cancer aligns with the “cues to action” part of the theory, where increased knowledge of the disease will likely have an effect on the perceived threat of breast cancer, increasing the likelihood of behavior change. This may also help promote the perceived benefits of breast cancer screening, also increasing the likelihood of choosing action (preventative measures). | Monthly educational courses will be provided to the public at the Clarkston Community Center |
| Provision of Mammogram Services and self breast examination training | Providing mammogram services through the community health clinic aligns with “cues to action”, as well as “perceived benefits” vs. “perceived barriers” through allowing greater access to prevention services and through increasing knowledge of the importance of these services | The Clarkston Community Health Center will be provided the necessary tools for mammogram screening, including training of individuals on interpreting the results. Community members will be made aware of this service which will be provided for free for those above 40 years of age or those who are otherwise considered susceptible to developing breast cancer. |
| Health Center reminders every 6 months for those above 40 years of age | This falls under the “cues to action” category as well, through encouraging women to continue performing breast cancer self examinations and mammograms where necessary. | Reminders should be sent out as text messages or as phone calls to women above the age of 40 in the Clarkston Community through the Community Health Center. |
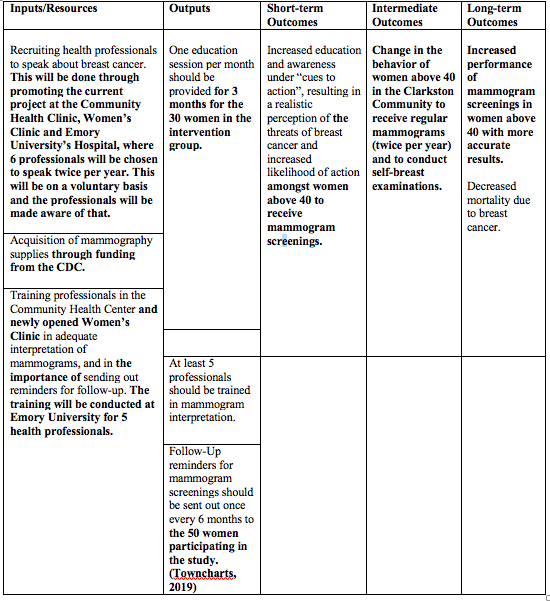
- Provide the logic model for the program as a schematic. (24 points)
- Explicitly state the causal and intervention hypotheses. You should have an intervention hypothesis linking each item in your activities to one or more short-term outcomes, and a causal hypothesis linking each item in short-term outcomes to at least one intermediate or long-term outcome. (12 points)
Intervention hypothesis example format: [Intervention activities] will lead to increases/decreases/improvements in [health behavior].
Intervention Hypothesis:
Provision of education through courses by health professionals will Increase knowledge about breast cancer screening/diagnosis/treatment amongst women in Clarkston City (18+) which will lead to increases in breast cancer screening behavior among women.
Provision of Mammogram Services and self breast examination training to women 18+ in the Clarkston Community, will increase the perceived benefits of performing mammograms/self breast exams, and will decrease the perceived barriers to these prevention measures, increasing the likelihood of women pursuing these diagnostic measures.
Providing Health Center reminders every 6 months for those above 40 years of age to receive mammogram screening tests will help increase “cues to action”, leading to an increased awareness of the dangers of breast cancer, and an increased likelihood for women to receive regular mammogram testing.
Causal Hypothesis:
Increasing the knowledge about breast cancer among women in the Clarkston Community will increase the perceived threat of disease, increasing the likelihood of women performing self breast examinations and pursuing mammogram testing, decreasing the incidence of breast-cancer related mortality in the long-term.
Goal 1: Increase knowledge of breast cancer prevention, diagnosis, threats, and treatment.
Outcome: A questionnaire about breast cancer in multiple languages will be distributed at the start of the educational program which will consist of 1 educational course per month for 3 months. The same questionnaire should be distributed at the end of the third session. We should see an overall increase in knowledge (significantly different increase in scores) in at least 20% of women attending the session. The questionnaire will be distributed again 3 months following the last session. (Dunn et. al, 2017)
Goal 2: Increase breast cancer screening rates amongst women 40 years + in the Clarkston Community.
Outcome: At the end of each education session, the attendants will be given information about receiving a free mammogram through the Women’s Clinic if desired. Women will have access to a free screening for up to 6 months following the last education session at their convenience. At least 30% of those who attended the education session should have received mammogram testing by 6 months following their educational session. A measure of those in the control group undergoing mammogram screening will be kept as well.
Part IV. Evaluation Design and Measures
- State the major stakeholders (minimum of 3) of your project, evaluation questions each stakeholder may want answered about the project, and how each group of stakeholders might be affected by the evaluation outcomes? Be sure to consider any individual or group who you list on your Inputs column of your logic model. (15 points)
| Stakeholder | Role in Intervention | Evaluation Questions from Stakeholder | Effect on Stakeholder of a Successful Program | Effect on Stakeholder of an Unsuccessful Program |
| Community Health Center | Provision of free mammography services | Will this program support our existing work/efforts to provide health care in the community? Will this program help prevent breast cancer in the Clarkston Community?Is this sustainable? | Better implementation of breast cancer awareness/screening strategies | No change in services offered and no change in mortality rates as a result of breast cancer |
| Women 40 yrs + in the Clarkston Community | Receivers of breast cancer educational training course, mammography service, breast self examination training | Wil my participation in this program help my overall health? Will my participation in this program improve my overall knowledge of breast cancer? | Better awareness/knowledge of breast cancer & the process of diagnosis/early detection/treatment; change in health behavior promoting regular screening for breast cancer and the encouragement of others to do the same; earlier detection of breast cancer in the community/prevention of mortality associated with breast cancer | No change in behavior regarding screening for breast cancer; stagnant mortality rate in the community as a result of breast cancer |
| Health Professionals | Receive training in order to adequately interpret mammography screening results Sending reminders to clients every 6 months to receive mammography screening | Am I adequately expanding my knowledge base about breast cancer, and accurately interpreting screening results as a result of the training received through this program? Am I getting positive results back from sending reminders to clients about receiving mammograms? | Better rates of mammography screening amongst women in the Clarkston Community. Gaining skills in mammogram screening interpretation. | Inadequate training in the field of screening interpretation. |
| Grant Providers | Supply money for the acquisition of mammography supplies, for training health professionals in screening interpretation, and in conducting program evaluations | Am I seeing a positive return in investment? Are we helping reduce the mortality due to breast cancer in the Clarkston Community? | Increased awareness of the incidence of breast cancer amongst women in the Clarkston community Lower rates of mortality due to breast cancer Earlier staging of breast cancer | No change in attitude/perception toward breast cancer screening Loss of profit over an unsuccessful program |
- Provide the outcome evaluation design(s) name and the scientific notation (Xs and Os). Name the major threats to internal validity for your evaluation, briefly describe why they are a threat, and discuss how your study design or other methods (e.g., incentives) will attenuate these threats. (21 points)
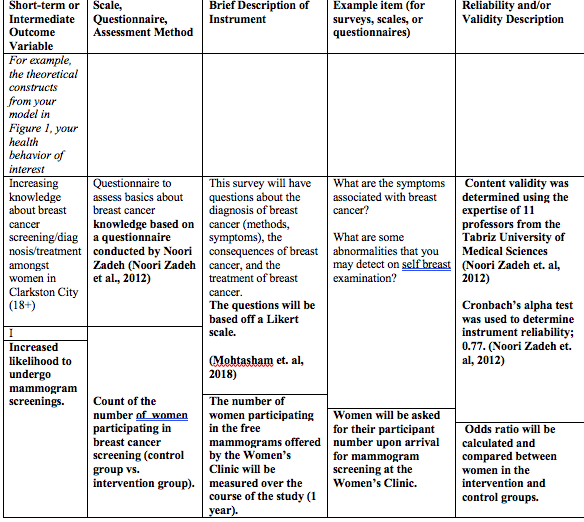
The outcome evaluation design will be a group randomized control trial. 50 women will participate in the overall study. The intervention group will consist of 30 women who will participate in the educational program and will have access to free mammogram screenings through the Clarkston Women’s Clinic. 20 women will make up the control group, who will have access to free mammogram screenings but will not attend the educational session. Both groups will undergo initial questionnaire in order to assess their general knowledge about breast cancer and their attitude/behavior toward breast cancer screening examinations. Both groups will be given the post-intervention questionnaire in order to assess knowledge gain in the intervention group. All participants will be chosen from the Clarkston Community with the requirement that they must be female and at least 40 years of age. An information session will be conducted about the program to be implemented, and the 50 women will be chosen randomly from those meeting the age and gender criteria, who participate in the information session.
R O1 TX O2 O3 (Intervention Group)
R O1 O2 O3 (Control Group)
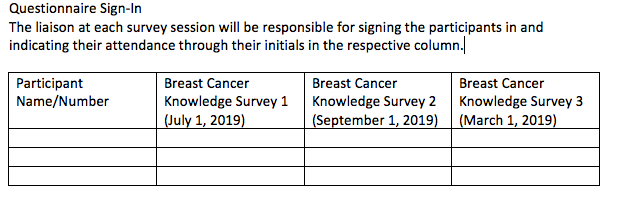
O1 = initial questionnaire
O2 = post-test at the end of the educational program
O3 = post-test 6 months after initiation of the study
A randomized control trial design will help minimize threats to internal validity. However, some threats include selection bias. Those who chose to come to the information session may have an interest in learning about breast cancer and may not be representative of the rest of the women above the age of 40 years in the Clarkston community. Another threat to internal validity includes attrition, and ensuring that the participants will engage in all aspects of the program including attending the educational sessions when required and receiving screening tests. Attrition will be detected through the questionnaires that are administered where the participants’ participation will be tracked using a participant number. In addition, attendance will be taken at each educational session. Testing bias is another threat to internal validity. Those who are selected for the control group may feel as if they are not benefitting as much from the program. We will emphasize the importance of the study in implementing an effective long-term program in the community to encourage participation. However, there may be participants in the control group who seek out their own breast cancer educational resources.
In order to evaluate the efficacy of the training of health professionals in screening interpretation, the health professionals will be required to have a mammogram film interpretation pre-test completed to test their accuracy in reading mammograms. They will then be subject to a film interpretation test consisting of pre-set films that have been previously interpreted and confirmed, following training, to ensure that they have met minimum standards in screening interpretation.
- You are putting together a survey to answer these outcome evaluation questions. Use the table to describe the variables you will measure and how. Be sure to include information on the validity and reliability of the instruments. You may see reliability reported as test-retest reliability or internal consistency (AKA: Cronbach’s alpha). Validity may be reported as face or content validity or construct validity (e.g., factor loadings). (20 points)
Part V. Process Evaluation and Data Collection Forms
- Provide the following data collection forms for monitoring the program process. More than one form may be submitted for a given category, but all forms must be clearly labeled. (18 points)
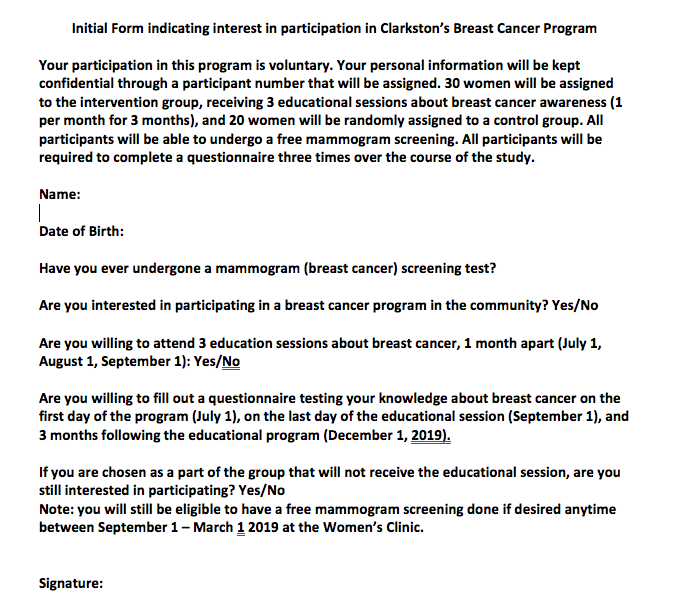
- Recruitment and enrollment – how will you track who you invite to participate in your intervention and who actually takes part?
Recruitment and enrollment:
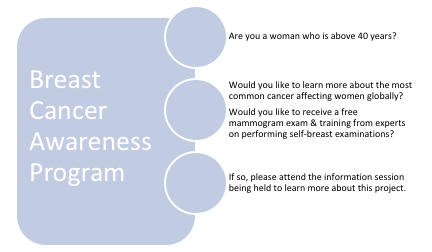
This flyer will be distributed throughout the Clarkston Community in multiple languages in order to reach as many women meeting the criteria as possible. Those who attend the information session will then fill out a form indicating their interest in participating in the program. Out of those, 50 women will randomly be chosen for the study. 30 participants will be placed in the intervention group, and 20 participants will be chosen for the control group.
- Attrition – how will you know if participants complete all of the observations (O’s from your study design) and all of the intervention components (from your Outputs column of your logic model)?
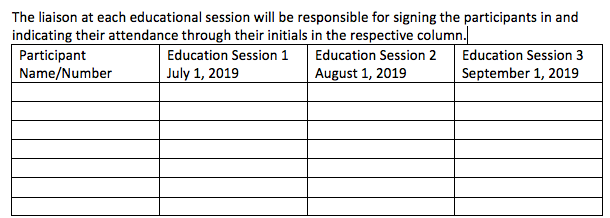
Participants will be asked to sign in at the beginning of each educational session and training session. Their names and information will be taken on intake at the Community Health Center upon administration of the mammogram screening examination.
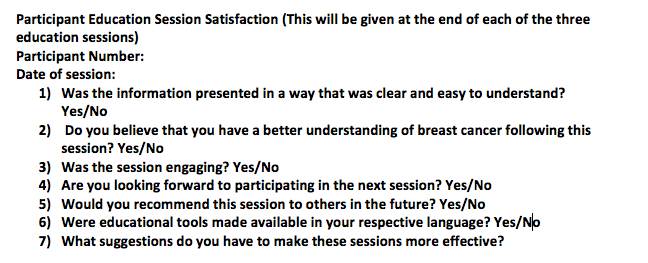
- Fidelity of the program – how will you know if the intervention was implemented as you had planned? This should match your Outputs column of your logic model.
The number of education sessions (once per month) conducted will be assessed through an appointed liaison who will be in charge of keeping track of the number of women attending the sessions, and the quality of the sessions conducted by trained health professionals.
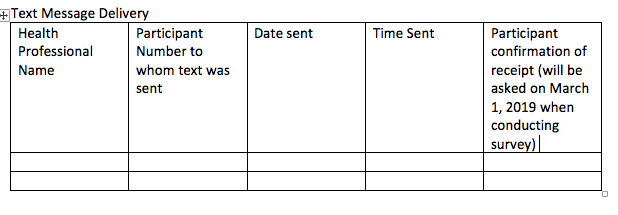
The number of reminders sent from the Community Health Clinic will be tracked through the text messages or calls that are conducted (health professionals will be asked to record their messages/time/date that they are sent and the recipients to whom they are sent).
References:
Arredondo, E. M., Haughton, J., Ayala, G. X., Slymen, D. J., Sallis, J. F., Burke, K., . . . Elder, J. (2015). Fe en Accion/Faith in Action: Design and implementation of a church-based randomized trial to promote physical activity and cancer screening among churchgoing Latinas. Contemp Clin Trials, 45(Pt B), 404-415. doi:10.1016/j.cct.2015.09.008
Darvishpour, A., Vajari, S. M., & Noroozi, S. (2018). Can Health Belief Model Predict Breast Cancer Screening Behaviors? Open Access Maced J Med Sci, 6(5), 949-953. doi:10.3889/oamjms.2018.183
Dunn, S., Lofters, A., Ophira M. Ginsburg, Christopher A. Meaney, Farah Ahmad, M. Catherine Moravac, Cam Tu Janet Nguyen, Angela M. Arisz,Cervical and Breast Cancer Screening After CARES: A Community Program for Immigrant and Marginalized Women. American Journal of Preventive Medicine. Volume 52, Issue 5 2017. https://doi.org/10.1016/j.amepre.2016.11.023.
Ghaffari, M., Rad, T. N., Mohammadi, S., & Rakhshanderou, S. (2018). Effect of an Intervention on the Breast Cancer Screening Behavior in Women: Application of Integrated Behavioral Model. International journal of preventive medicine, 9, 99. doi:10.4103/ijpvm.IJPVM_147_17
Kaplan, J., DeSimone, M., Phan Le, T.-L., Newman, S., & Goedken, J. (2018). Delivering Health Care to Refugee and Immigrant Women in Clarkston, GA: Opening a Women’s Clinic [28M]. Obstetrics & Gynecology, 131, 148S. Retrieved from https://journals.lww.com/greenjournal/Fulltext/2018/05001/Delivering_Health_Care_to_Refugee_and_Immigrant.514.aspx. doi:10.1097/01.AOG.0000533084.86971.e2
Noori Zadeh R, Bakhtiary Aghdam F, Sahebi L. Knowledge, health beliefs and breast cancer screening behaviors of women referring to health centers of Tabriz 2010. Iran J Breast Dis 2010;3:43‐51. TownCharts. “Clarkston, Georgia Demographics Data”. 2019. https://www.towncharts.com/Georgia/Demographics/Clarkston-city-GA-Demographics-data.html