BY STELLA NWOSU
GLOBAL HEALTH CERTIFICATE COURSE (GLOB 7100)
Abstract
Rwanda is one of the smallest countries on the African mainland, its capital city is Kigali. Rwanda has made impressive progress in improving health outcomes. The major challenges/gaps in the health sector of Rwanda include: Increasing cases of non-communicable diseases(NCDs), Malaria is still endemic in Rwanda, Tuberculosis, Malnutrition, Shortage of workforce (Both clinical and management), Infrastructure development and Self-sufficiency in pharmaceuticals production. The top five causes of DALYs (Fig.1) are : Maternal & Neonatal diseases, Respiratory Tract Infections & Tb, Cardiovascular Diseases, NTDs &Malaria and Other Non-Communicable Disease . the top five causes of mortality (Fig.2) are, Cardiovascular diseases , Respiratory Tract Infections & TB , Neoplasms Maternal and neonatal disorders and Digestive diseases . The country has attained the Abuja declaration of allocating 15% of the government budget allocated to health, and established a functional and affordable health insurance system for households. Coverage of health insurance currently stands at 83.6% of the population for CBHI (as of June 2017) and at 90% if all health insurance schemes are included. However, there is still some work to be done in the Rwanda health sector. The following recommendations would be of great benefit: Improved funding for the health sector, Increased workforce development, more infrastructural development and Health education to reduce the incidence of NCDs and other health challenges in the country. Rwanda has translated its policy intentions into a set of comprehensive and complementary actions embedded in a culture of performance management that has actually resulted in an increase in performance.
Introduction
Rwanda (Government of Rwanda: Welcome to Rwanda) is a landlocked country in the Great Rift Valley, where the African Great Lakes region and East Africa converge. One of the smallest countries on the African mainland, its capital city is Kigali. Located a few degrees south of the Equator, Rwanda is bordered by Uganda, Tanzania, Burundi, and the Democratic Republic of the Congo (Plate 1).

Plate 1: Administrative Map of Rwanda
(Source: http://www.google.com)
Rwanda has a population of over 12.6 million (United Nations- List of Countries by Population) living on 26,338 km2 (10,169 mi2) of land, and is the most densely populated mainland African country with 85% of its population living in rural areas. Rwanda has five provinces which are divided into 30 districts with each district being served by community health workers.
Rwanda’s Health Indicators
| HEALTH INDICATORS | 2009 | 2019 |
| Population Size | 9.24 million | 12.63 million |
| Life Expectancy at Birth | 58.92 years | 68.75 years |
| Neonatal Mortality Rate | 47.5/1,000 Live births | 26.3 / 1,000 Live births |
| Infant Mortality Rate | 47.5/1,000 Live births | 26.3/1,000 Live births |
| Under 5 Mortality | 70.7 / 1,000 Live births | 34.3/ 1,000 Live births |
| Maternal Mortality Ratio | 424/100,000 Live births | 248/100,000 Live births |
| The major challenges/gaps in the health sector of Rwanda include: Increasing cases of non-communicable diseases(NCDs)Malaria is still endemic in RwandaTuberculosisMalnutrition Shortage of healthcare workforce (Both clinical and management)Infrastructure development Self-sufficiency in pharmaceuticals production According to a web-based data bank on health (https://vizhub.healthdata.org/gbd-compare/ 5 Main Causes of DALYS & Main Causes of Death (2019) 1 Maternal& Neonatal disease Respiratory Infections and TB 2 Respiratory Tract Infection Cardiovascular diseases 3 Cardiovascular diseases Maternal & Neonatal diseases 4 Neglected Tropical disease& Malaria Neoplasm 5 Other Non-communicable disease Digestive diseases The population most impacted include; Those living with HIV, Poor women who are head of households, Out of school youths, orphans and vulnerable children. However the ‘Twiyubake’ project funded by USAID/PEPFAR and implemented in 12 districts of Rwanda to improve the health, nutrition and wellbeing on this population. According to the IHME website, the most common causes of death in women are; HIV&STIs, Neoplasms, Maternal&Neonatal diseases, Respiratory and Cardiovascular diseases. Women appear to be more significantly burdened by HIV&AIDS in Rwanda. Recent studies have shown that different factors such as rape, other related physical violence may have contributed to the numerous unhealthy physical and mental health impacts regarding HIV&AIDS on women. In the last 10 years Rwanda’s Maternal mortality rate has been steadily declined from 945(data.Worldank) in 2005 to 297 in 2015 per 100,000 Live births. Although Birth rate in Rwanda stands at 29.8 births per 1000 population (2018 est.), country 39th in the world, Total fertility rate is 3.75 children born/woman (2018 est.), the 41st in the world. |
Fig.1: 2019 DALYs Per100,000 population
(Source: https://vizhub.healthdata.org/gbd-compare/)
Fig.2: 2019 Causes of Mortality Per 100,000 population
(Source: https://vizhub.healthdata.org/gbd-compare/)
Critical Analysis of Health Systems Building Blocks
WHO framework that describes health systems in terms of six core components of “Building Blocks” (Fig.1):
- Service delivery,
- Health workforce,
- Health information systems,
- Access to essential medicines,
- Financing, and
- Leadership/Governance.
The six building blocks contribute to the strengthening of health systems in different ways (WHO, Monitoring the Building Blocks of Health Systems, 2010).
Fig.1: The World Health Organization’s Building Blocks of a Health System
(Source: Author’s Adaptation of the WHO Building Blocks of Health Systems)
- Health Service Delivery
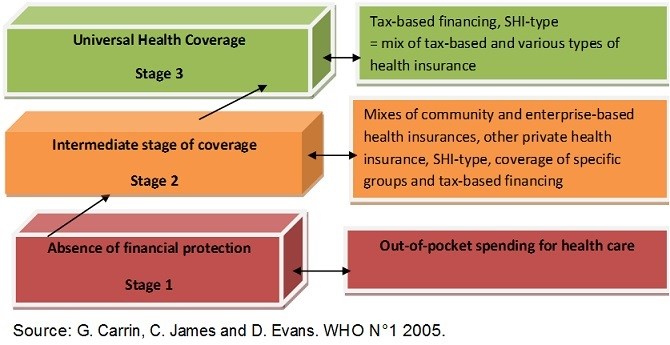
The WHO definition of Universal health coverage integrates 3 dimensions which are; equity in access to healthcare, quality of health services and financial risk protection. By 2009, the Rwandan government has made effort to develop its healthcare system in national and community level and has improved access to primary health services mainly through infrastructure development and expansion of a community-based health insurance program by creating the Mutuelle de Santé health insurance program, which provides access to basic primary health care services for 85% of its citizens (Lu, Chin, Lewandowski, Basigna, Hirshhom, Hill, Murray and Binagwaho, 2012). The transition of Rwanda UHC begins from Stage 1 – Stage 3.
Geographic access to care is relatively well distributed, with 75% of the nation’s population living within 5 kilometers of a health facility (Africa Health Workforce Observatory,2009). Although Rwanda is categorized a low income country by the World bank, Near universal coverage has been achieved due to strong political commitment, a decentralized and strong network of health facilities in all districts, and community participation. And so Rwanda has attained a Universal Health Coverage Index of 57(data.Worldbank) which seems fair compared to other countries in Sub-Saharan Africa.
Nevertheless, there has been marked shortage of trained health care workers with 0.04 generalist physicians and 0.62 nursing professionals per 1,000 people (Africa Health Workforce Observatory,2009) with community health workers making up an integral part of the health system.
- Information
The Rwanda Health Management Information System(HMIS) was established in 1998 with the goal to improve the quality of routinely-collected health data from community health workers (CHWs) and all Health Facilities across the country ,In 2008, the Rwanda Ministry of Health upgraded the HMIS to an electronic based system known as the District Health Information System version 2 (DHIS2) (Republic of Rwanda. Data Quality Assessment Procedures Manual, 2016). This system allows data to be stored centrally and easily accessed and maintained by facilities. Assessments by WHO revealed that the quality of the Rwanda HMIS data is high, regarding completeness and internal consistency of reported data for studied HMIS indicators (Nisingizwe, Iyer et al 2014). However, findings from two small-scale studies that tried to compare HMIS data and records in source documents, using a reporting accuracy definition different to the WHO data verification definition, suggest a variable level of agreement between HMIS data and records in source documents (Mitsunaga, Hedt-Gauthier, et al, 2015; Karengera, Govule, et al 2016].
- Financing
In almost two decades, the Rwandan government has increased its per capita spending on health from $16.94 in 2003 to $58 per capita in 2018( data.Worldbank)which exceeds the amount recommended by WHO ($34) for a country to be able to provide basic health services to its population. Following 2006, The performance based financing policy was implemented to strengthen the healthcare delivery. Through the PBF, payments are made to health facilities based on performance contracts and also provides incentives /rewards for healthcare providers to ensure high quality services, and accountability for the health system.
Despite the impressive performance registered in Rwanda concerning UHC and (UHI), the CBHI financial deficit has become chronic from 2011/2012 until now. As a result, every year the Government of Rwanda is obliged to intervene in the payment of CBHI debts to health facilities and this raises the question of whether the Rwanda CBHI is financially sustainable, so there is an urgent need to assure financial sustainability by identifying indicative alternative funding mechanisms and accompanying measures to support them strategically.
While making significant steps in improving Rwanda’s health status, the health sector remains heavily dependent on Rwandan government and external sources . External assistance is estimated to be roughly 61% of total public spending on health (NHA,2010).
- Human Resources
In 2011, Rwanda had 625 physicians, 8273 nurses, and 240 midwives providing care at 4 referral hospitals, 41 district hospitals, and 442 health centers (Rwanda Health Statistics Booklet, 2011). With a combined health-service provider density of 0.84 physicians, nurses, and midwives per 1000 population, Rwanda falls far below the minimum level recommended by the World Health Organization (WHO) of 1.5 providers per 1000 population. Approximately 45,000 community health workers across the 14,837 villages in Rwanda offer basic empirical diagnosis and treatment services, in addition to general health promotion, and they have been instrumental in the control of infectious diseases and the reduction of costs. Until 2012, most of the physicians in Rwanda were trained as generalists, and more than 90% of the nurses have the lowest level of nursing training available (equivalent to secondary-school qualifications, or A2 level). Access to specialists is generally limited to the two university hospitals and other facilities in Kigali, the capital.
While staff, particularly doctors, have been in short supply historically, there is steady increase in number of physician graduates. (Lewis, 2019).
According to Lewis, “A built-in phenomenon in healthcare is that supply creates demand, since it is physicians who create demand for healthcare on behalf of patients. The number of physicians in Rwanda currently is insufficient, and a gradual increase is likely warranted. However, according to the Medical Council, the historical number of physician graduates at the University of Rwanda (UoR) is about 100 per year. In a scale-up, that number will reach 379 in 2019. At the same time, three new medical schools are opening, and in the first year they together expect to graduate roughly 200 physicians (Lewis, 2019).
- Medicine and Technologies
Essential medicines are intended to be available within the context of functioning health systems at all times, in adequate amounts, in the appropriate dosage, with assured quality, and at a price that individuals and the community can afford (WHO,2005).
According to a report “Rwanda is set to become the first country in the world to have a digital-first universal primary care service, due to a government collaboration with Babylon Health. Allie Nawrat explores the transformation this African country has been through to make it a good location for implementing digital health innovations to benefit of its citizens” (https://medicaltechnology.nridigital.com/medical_technology_jun20/rwanda_digital_health)
“Another area of focus for Rwanda is technology. As part of nationwide digitization efforts, the government has invested in a broadband infrastructure that now covers 90% of the country and mobile phone penetration has exceeded 75% of the population. This is a particularly impressive feat since most of Rwanda’s 12.5 million people are spread out in rural areas with incredibly difficult topography” (https://medicaltechnology.nridigital.com/medical_technology_jun20/rwanda_digital_health).
The government also worked with Partners in Health to develop electronic health records (EHR) for HIV patients and services in 2005; this has now been extended to include all clinical records.
Building on Rwanda’s strong foundations in healthcare and technology – and to advance progress towards the country’s long-term development goals – the government signed a ten-year collaboration with UK-headquartered remote consultations provider Babylon Health. Together they will create the world’s first digital-first universal primary health care service, in which everyone over the age of 12 in Rwanda will have access to consultations with doctors or nurses through their mobile phones within minutes (https://medicaltechnology.nridigital.com/medical_technology_jun20/rwanda_digital_health).
In Rwanda, the pharmaceutical sector heavily relies on imports, In 2019, they spent around $ 97.6 million on drugs import alone, and it is expected to increase by $102.5 million in 2024 (http://www.fitch solutions.com/corporates/healthcare-pharma/rwanda-pharmaceutical-exportsincrease-domestic-industryexpands-09-09-2020).
About 20% of these import expenses are expected to be reduced by the establishment of the first pharmaceutical factory in the country (The New Times, Rwanda, 2017). Public and private sectors preserve the drug supply chain in Rwanda.
- Leadership and governance
Much has been said and written about Rwanda’s remarkable achievements in the domain of health. The government’s interest in decentralization of the health system has led to an improvement in health service delivery. In 2008, all healthcare facilities were granted financial and administrative autonomy in other for the smooth running of the performance based finance initiative. Several articles published in prestigious journals (Binagwaho et al., 2013), (Farmer et al.,2013), (Bucagu et al.,2012) and (Logie et al.,2008) links the improved performance to governance—including donor coordination and the alignment of external aid to government policy—as well as to concrete initiatives such as community health insurance (mutuelles de santé) and performance-based financing (PBF). It is the district heath managers who are the key agents leading district health teams and supervising hospital staff so as to achieve targets and contribute to better overall health sector performance.
Table 1: WHO’s Building Blocks of a Health System.
| BUILDING BLOCK | RATING | COMMENT |
| Health Service Delivery | Very Good | Service delivery is on the high side but more still need to be done |
| Information (Health Information Systems ) | Very Good | Recent assessments revealed that the quality of the Rwanda HMIS data is high |
| Finance (Health Care Financing) | Fair | External assistance is estimated to be roughly 61% of total public spending on health |
| Health Work Force | Fair | While staff, particularly doctors, have been in short supply historically, there is rapid growth of physician graduates, with the number increasing by almost 400 percent this year. |
| Medicine and Technologies | Good | The government also worked with Partners in Health to develop electronic health records (EHR) for HIV patients and services in 2005; this has now been extended to include all clinical records |
| Leadership and Governance | Very Good | the government signed a ten-year collaboration with UK-headquartered remote consultations provider Babylon Health. Together they will create the world’s first digital-first universal primary health care service, in which everyone over the age of 12 in Rwanda will have access to consultations with doctors or nurses through their mobile phones within minutes |
(Source: Author’s Adaptation of the WHO building Blocks of a Health System)
Effective Health Interventions
The Rwanda Vision 2020 considers health finance accessibility as a key priority of its strategic direction. The current health financing sustainability policy is aligned with the Health Sector Policy of 2015 (Health Sector Policy,2015) and the second Economic Development and Poverty Reduction Strategy, which aims to develop a wide-ranging financing framework for health systems based on best practices in global health care financing. This framework is built on two main pillars: (a) on the supply side, the implementation of fiscal decentralization with increased transfers from central government to local governments and peripheral health facilities on the basis of needs and performance; (b) on the demand side, the establishment of a health insurance system including cross-subsidies from higher-income to lower-income populations (Mid Term Review of the Rwanda HSSP3, 2015). These mechanisms have enabled achievement of a number of major health sector targets, including reduction of unmet needs, increased use of health care services, decreased incidence of catastrophic health expenditures and decreased inequality in access to health care services. Progress has been facilitated by political commitment and development of a legal framework that made health insurance compulsory for all Rwandans.
The country has attained the Abuja declaration of allocating 15% of the government budget allocated to health, and established a functional and affordable health insurance system for households. Coverage of health insurance currently stands at 83.6% of the population for CBHI (as of June 2017) and at 90% if all health insurance schemes are included. The introduction of Performance Based Financing (PBF) has yielded efficiency gains for the health system.
There is still some work to do in the Rwanda health sector. The following recommendations would be of great benefit:
- Improved funding for the health sector
- Increased manpower development
- More infrastructural development
- Health education to reduce the incidence of NCDs and other health challenges in the country.
Conclusions
Rwanda has translated its policy intentions into a set of comprehensive and complementary actions embedded in a culture of performance management that has actually resulted in an increase in performance. There is a strong political will by the government of Rwanda to improve the health care system of the country. The referral system is so efficient that access to healthcare is almost guaranteed for all Rwandans. There is a high uptake of the Community Based Health Insurance (CBHI) system in the country, hence meeting universal health coverage targets. Rwanda remains the beacon of health care delivery in Africa. However, the country still grapples with high levels of Chronic diseases, Malaria and Tuberculosis and other infectious diseases. More still need to be done to attain full coverage and a near perfect heath care system.
References:
Andoh-Adjei, F. X. (2018, August 27). Effects of capitation payment on utilization and claims expenditure under National Health Insurance Scheme: a cross-sectional study of three regions in Ghana. Retrieved May 5, 2021, from https://healtheconomicsreview.biomedcentral.com/articles/10.1186/s13561-018-0203-9
Basinga, P. (2011, April 23). Effect on maternal and child health services in Rwanda of payment to primary health-care providers for performance: an impact evaluation. Retrieved May 5, 2021, from https://pubmed.ncbi.nlm.nih.gov/21515164/
Binagwaho, A. (2014, July 26). Rwanda 20 years on: investing in life. Retrieved May 5, 2021, from https://pubmed.ncbi.nlm.nih.gov/24703831/
Bucagu, M. (2012, June). Impact of health systems strengthening on coverage of maternal health services in Rwanda, 2000–2010: a systematic review. Retrieved May 5, 2021, from https://pubmed.ncbi.nlm.nih.gov/22789082/
Carrin, G. (2002, December 19). Social health insurance in developing countries: A continuing challenge. Retrieved May 5, 2021, from https://onlinelibrary.wiley.com/doi/abs/10.1111/1468-246X.00124
Countdown to 2015. (n.d.). A Decade of Tracking Progress for Maternal, Newborn and Child Survival The 2015 Report. Retrieved May 5, 2021, from http://www.countdown2015mnch.org/wp-content/uploads/2017/11/CDReport_2015_ex-profiles_final.pdf
Farmer et.al, P. E. (2013, January 8). Reduced premature mortality in Rwanda: lessons from success. Retrieved May 5, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3548616/
Fitch Solutions / Healthcare & Pharma. (2020, September). Rwanda Pharmaceutical Exports To Increase As Domestic Industry Expands. Retrieved May 5, 2021, from https://www.fitchsolutions.com/corporates/healthcare-pharma/rwanda-pharmaceutical-exports-increase-domestic-industry-expands-09-09-2020
GBD 2017 DALYs and HALE Collaborators. (2018, November 10). Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the global burden of disease study 2017. Retrieved May 5, 2021, from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)32335-3/fulltext
GHWA, WHO, Africa Health Workforce Observatory. (n.d.). Human resources for health country profile template tool. Retrieved May 5, 2021, from https://www.who.int/workforcealliance/knowledge/toolkit/2/en/
Gosden, T. (2000). Capitation, salary, fee-for-service and mixed systems of payment: effects on the behavior of primary care physicians. Retrieved May 5, 2021, from https://pubmed.ncbi.nlm.nih.gov/10908531/
Government of Rwanda Ministry of Health. (n.d.). THIRD HEALTH SECTOR STRATEGIC PLAN. Retrieved May 5, 2021, from http://www.diplomatie.be/oda/18553_PROGDESCR_HSSP_III_FINAL_VERSION.pdf
IGC International growth center. (n.d.). Addressing efficiency and quality in Rwanda’s health system. Retrieved May 5, 2021, from https://www.theigc.org/wp-content/uploads/2020/01/Lewis-2019-final-paper.pdf
IHME GHDx. (n.d.). Rwanda Health Statistics Booklet 2011. Retrieved May 5, 2021, from http://ghdx.healthdata.org/record/rwanda-health-statistics-booklet-2011
LIU, K. (2018, May 10). Decomposing health inequality with population-based surveys: a case study in Rwanda. Retrieved May 5, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5946429/
Logie, D. E. (2008, July). Innovations in Rwanda’s health system: looking to the future. Retrieved May 5, 2021, from https://pubmed.ncbi.nlm.nih.gov/18619670/
Lu, C. (2012, June 18). Towards Universal Health Coverage: An Evaluation of Rwanda Mutuelles in Its First Eight Years. Retrieved May 5, 2021, from https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0039282
Maiiga, A. (2019, September 29). Generating statistics from health facility data: the state of routine health information systems in Eastern and Southern Africa. Retrieved May 5, 2021, from https://pubmed.ncbi.nlm.nih.gov/31637032/
Ministry of health. (n.d.). HEALTH SECTOR POLICY 2015. Retrieved May 5, 2021, from https://www.moh.gov.rw/news-detail/health-sector-policy-2015
Murray, C. (n.d.). Health systems performance assessment : debates, methods and empiricism / edited by Christopher J. L. Murray, David B. Evans. Retrieved May 5, 2021, from https://apps.who.int/iris/handle/10665/42735
Nisingizwe, M. P. (2014a, November 19). Toward utilization of data for program management and evaluation: quality assessment of five years of health management information system data in Rwanda. Retrieved May 5, 2021, from https://www.tandfonline.com/doi/full/10.3402/gha.v7.25829
Nshimyiryo, A. (2020, July 17). Health management information system (HMIS) data verification: A case study in four districts in Rwanda. Retrieved May 5, 2021, from https://pubmed.ncbi.nlm.nih.gov/32678851/
Nyandekwe, M. (2014, March 27). Universal health coverage in Rwanda: dream or reality. Retrieved May 5, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4145275/
Nyandekwe, M. (2020, September 14). Universal health insurance in Rwanda: major challenges and solutions for financial sustainability case study of Rwanda community-based health insurance part I. Retrieved May 5, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7648486/
Nyatanyi, T. (2017, February 21). Implementing One Health as an integrated approach to health in Rwanda. Retrieved May 5, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5335763/
Republic of Rwanda Ministry of Health. (2013, November). ANNUAL REPORT July 2012-June 2013. Retrieved May 5, 2021, from https://extranet.who.int/countryplanningcycles/sites/default/files/planning_cycle_repository/rwanda/moh_annual_report_july_2012-june_2013.pdf
Republic of Rwanda Ministry of Health. (2015, March). Health financing sustainability policy. Retrieved May 5, 2021, from https://www.moh.gov.rw/fileadmin/user_upload/policies/Health_Financing_Sustainability_Policy_March_2015.pdf
Rich, M. L. (2012, March 1). Excellent clinical outcomes and high retention in care among adults in a community-based HIV treatment program in rural Rwanda. Retrieved May 5, 2021, from https://pubmed.ncbi.nlm.nih.gov/22156912/
Rwandan research and implementation writing group. (2014, January). Building health research infrastructure in Rwanda. Retrieved May 5, 2021, from https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(13)70144-X/fulltext
The Newtimes. (2017, December 16). Pharmaceuticals factory to reduce 20% of Rwanda’s drug imports. Retrieved May 5, 2021, from https://www.newtimes.co.rw/section/read/225685
World Health Organization. (n.d.-a). Essential medicines and health products. Retrieved May 5, 2021, from https://www.who.int/medicines/services/essmedicines_def/en/
World Health Organization. (n.d.-b). Framework and Standards for Country Health Information Systems Second edition. Retrieved May 5, 2021, from https://www.who.int/healthinfo/country_monitoring_evaluation/who-hmn-framework-standards-chi.pdf
World Health Organization. (n.d.-c). Previous reports press kit the world health report 2006 – working together for health. Retrieved May 5, 2021, from https://www.who.int/whr/2006/en/

