What is happening?
The Chinese government has started collecting the genetic information of Uighur Muslims, an ethnic minority group in Western China. This is happening while the Chinese government is currently detaining as many as 1 million people in internment camps. Although they claim they have not been hurting them, there is much speculation as to what the Chinese government is doing in these camps(5). They claim they are using the camps to re-educate the Muslims and assimilate them into Han Chinese culture, very similar to the Native American internment camps that the United States and Canada used to have. To collect the Uighur DNA, the Chinese government will make the population come in for mandatory health checks, where they will then draw their blood and use that to collect and store their genetic information without their consent. In many cases, they were strongly coerced into giving up their genetic information(3).
What technology is being used?
The DNA being collected is primarily used to distinguish between ethnic groups. Uighur DNA is compared to samples from other ethnicities. The DNA is genetically compared using microarray-based autosomal DNA testing(3). Paternal ancestry is tracked by looking at the y chromosome while maternal DNA is tracked by looking at mitochondrial DNA. The genomes collected are then parsed up into pieces or separate SNPs or haplotypes. They then compare the haplotypes in the sample to haplotypes from a database, which allows them to see in which ethnicities these haplotypes are most common and match the DNA sample to the ethnicity it most likely came from based on its genetic information(2).
Where are they getting this technology?
China got their technology from the United States company Thermo-Fisher. Thermo-Fisher sells lab equipment, DNA testing kits, and DNA mapping machines to help scientists determine a person’s ethnicity and identify diseases they are susceptible to. China accounted for 10% of Thermo-Fisher’s revenue. In addition, genetic information to use to compare to Uighur DNA was provided by Yale geneticist Kenneth Kidd(3).
What are the uses of this technology?
This genetic technology has been widely used not only by China. In the United States, it can be used to track down criminals. If a family member gives their genetic information to databases like 23 and me, the US government can then use that family member’s data to trace criminals and solve crimes that were unsolvable before(5). Many people are glad that this technology exists to catch criminals, but issues like those in China raise issues on the ethical issues that might arise if this technology is used for the wrong reasons(3).
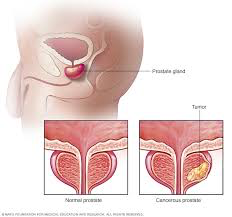
Why are they collecting this data?
In patents filed in 2017, the Chinese stated that they are collecting this data to help them determine the geographical origin of criminals by collecting DNA samples from the crime scene. They also cite this as a way to stop terrorism(3). The government has had a long history of treating Uighurs as a threat. Many Chinese citizens believe that they are terrorists, and they have been accused of many violent acts of terrorism throughout this decade. They put them in internment camps to try to ensure that they remain loyal to the Chinese government(3). The Chinese say they are collecting this DNA database to track any Uighur Muslims that try to leave the detainment camps.
What issues does this raise in general?
Many scientists are worried about the fact that the Chinese government entered the Uighurs genetic information into a global database when they are not sure that their data collection was consensual. This violates many privacy concerns, both in the scientific community and abroad(1). It is also a big issue that the Chinese government could be using this technology to keep an entire population trapped with no way to escape.
Parallels in United States?
What happens if the United States citizens DNA ever got into the hands of the wrong people. Even though now, the government has special privacy protections, if that ever changed, the DNA on file is permanent and can easily be abused. In addition, many companies that collect DNA, like 23 and me, do not reveal who they give the DNA to, so users are at risk. They also do not compensate those who give their DNA for adding their DNA to global databases. Especially with online data theft, this is especially a concern. There are some benefits, such as catching criminals or individual benefits such as determining what diseases people may be at risk for, so they can take preventative measures. However, even in the United States, there are discussions about the possible risks(1).
What issues does this raise for the United States?
Dr. Cavlan stated, “Honestly, there’s been a kind of naïveté on the part of American scientists presuming that other people will follow the same rules and standards wherever they come from,”. This is very accurate. Even though Americans or other western countries create new technology and develop rules to regulate its use, often times this technology can get into the hands of countries who do not have the same standards, and it can be used to fuel genocide or other human rights violations(5). This is important as developed countries begin to create more high-tech genetic tests that can be used in other ways to violate human rights. The United States and other developed nations should ensure that they are protecting these tests or at least ensure that people worldwide are not being oppressed using this technology.
Should people be held accountable?
Thermo Fisher says they were unaware of what China was using the technology for, and they have also agreed to stop selling their technology to Xinjian province, where the DNA collection is happening. In addition, Kidd says he thought the Chinese were following the worldwide norm of requiring consent to collect DNA(3). However, they still contributed to human rights violations with no repercussions. There should be a significant discussion as to whether or not they should be held responsible for the repercussions of their contributions.
Why is this important?
As these technologies develop, it is important to consider their ramifications and effects. Even if the United States or other western countries have some form of regulation, often other countries do not. The Uighur Muslims are just one example of the potential for genetic testing to be used to oppress different groups. It is important to consider how we as citizens can work ourselves and also hold our governments accountable for ensuring that these technologies do not violate any human rights. This is important both for the sake of helping others but also for protecting ourselves in the future.
Works Cited:
- AncestryDNA® – Frequently Asked Questions (United States). (n.d.). Retrieved November 14, 2019, from https://www.ancestry.com/dna/en/legal/us/faq#about-3.
- Curtis, R. (2015, May 5). AncestryDNA | Breaking Down the Science Behind Ethnicity Results | Ancestry. Retrieved December 1, 2019, from https://www.youtube.com/watch?v=o0mVUu2kRcs.
- Haas, B. (2017, December 13). Chinese authorities collecting DNA from all residents of Xinjiang. Retrieved November 14, 2019, from https://www.theguardian.com/world/2017/dec/13/chinese-authorities-collecting-dna-residents-xinjiang.
- Raven, K. (2018, November 18). Is an At-Home DNA Test an Ideal Gift, Really? Retrieved November 14, 2019, from https://www.yalemedicine.org/stories/at-home-genetic-test-kit-holiday-gift/.
- Wee, S.-lee. (2019, February 21). China Uses DNA to Track Its People, With the Help of American Expertise. Retrieved November 14, 2019, from https://www.nytimes.com/2019/02/21/business/china-xinjiang-uighur-dna-thermo-fisher.html.