What is the Trait Being Tested?
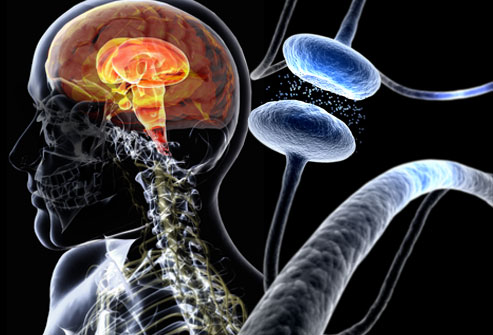
Parkinson’s disease is here and affecting many people’s lives. It’s the runner-up neurodegenerative disorder making it the second most common disease next to Alzheimer’s disease. In North America alone, more than one million people are affected by it. Parkinson’s disease is distributed among “1% of 55-year-olds and more than 3% of those over age 75”. Altogether, there are more than four million people with PD worldwide(6).
There are 18 chromosomal regions involved in Parkinson’s. However, “[not] all of the identified genes contain causative or disease-determining mutations”(4). For example, alterations in GBA and UCHL1, “do not cause Parkinson disease but appear to modify the risk of developing the condition in some families”(5). The names of the regions are numbered chronologically from PARK1 to PARK18. These names are really nick-names of the underlying regions. For example, PARK6 is really PINK1. Relating to the genes, “we know of 28 distinct chromosomal regions more or less convincingly related to PD. Only six of these specific regions contain genes with mutations that conclusively cause monogenic PD” or “a form of the disease for which a mutation in a single gene is sufficient to cause the phenotype”(4). NIH states that “variations in other genes that have not been identified probably also contribute to Parkinson’s disease risk”(5).
Specifically, “Familial cases of Parkinson’s disease can be caused by mutations in the LRRK2, PARK7, PINK1, PRKN, or SNCA gene, or by alterations in genes that have not been identified”. However, mutations of these genes can happen to people who have not inherited the disease and the causes of these sporadic mutations are unknown. The functions of all the proteins generally are producing dopamine in the “substantia nigra”(5). Therefore, these proteins are a part of dopamine-producing neuron cells and are made in these specific neuron cells. Because these genes produce proteins that produce dopamine, it makes sense that an alteration, variation, or change in the structure of these proteins would lead to a lack of dopamine production in the brain, thus leading to the trait of Parkinson’s disease.
Why Get Tested?
Genetic testing for Parkinson’s disease has not been formalized under either the “Movement Disorder Society or any other PD alliance group”. Testing is encouraged for those with “juvenile-onset PD irrespective of family history; early-onset PD with atypical features and/or a positive family history of this disease; or late-onset PD with a strong family history of PD”. Genetic testing is strongly recommended for patients with early-onset PD. This is to help these people “understand their disease and to make informed life decisions”. It has been argued that testing would not change the clinical management of Parkinson’s. However, according to a journal by Christine Klein and Ana Westenberger(4) that is published on pubmed.gov, testing is becoming exceedingly more important in identifying mutations that will lead to more effective treatment routes(4). If the patient wants more effective treatments, testing is a viable option. It is important for understanding how family plays a role in PD. To start, only fifteen percent of those with PD have a family history with ten percent being reported from other sources(5). However, it is still important for those who have relatives with PD to understand how the disease spread through their family. The genes that spread through a family are the aforementioned LRRK2, PARK7, PINK1, PRKN, and SNCA genes. Furthermore, genes that affect Parkinson’s disease are (1) autosomal dominant, (2) autosomal recessive, and (3) autosomal dominant with reduced penetrance. “In clinical practice, however, pedigrees rarely follow that aforementioned well-defined Mendelian inheritance patterns, i.e., they are frequently complicated by reduced penetrance, variable expressivity, and phenocopy phenomena”(4). Because of this and the variability of inheritance patterns across the genes that lead to PD, it is important for people to be aware of family history in order to make an informed decision about testing for PD.
For those who decided to test for PD, I recommend a single-nucleotide polymorphisms test in order to determine whether you have certain variants that “are considered to be [associated] with the disease”(4). The cost to test for all six known genes would cost $4,000 and would not be covered by Medicare(1). The type of test recommended given for the most common alleles for Parkin. Parkin mutations account for “77% of the familial cases with an age of onset [less than thirty years] (Lucking et al. 2000), and for 10%–20% of patients in general”. In addition to Parkin, LRRK2 and PINK1 are more common monogenic forms in which testing is recommended. However, testing is generally discouraged for those without “juvenile-onset PD irrespective of family history; early-onset PD with atypical features and/or a positive family history of this disease; or late-onset PD with a strong family history of PD” as mentioned previously(4). Moreover, there is good evidence supporting a connection between these variations and the trait in question in cases where “many family members affected by Parkinson’s disease”(7). The base risk of PD increases with age as PD typically develops in middle to late life. After identifying the variation, the person’s actual risk is not significantly increased unless the person has a family history of the disease.
Think Before You Spit:
There are scientific reasons that someone should not test for PD. There are no diagnostic criteria for SNPs for PD and therefore should avoid testing unless PD is prominent in the family. Risks of misdiagnosis are increased when these types of tests are taken because of a lack of conclusiveness. “Because there is no conclusive screening or test, patients with very early Parkinson’s disease may not meet the clinical diagnosis criteria. On the flip side, this lack of specificity means that you could be diagnosed with Parkinson’s disease, only to find out later that you have a different condition that mimics Parkinson’s”. Instead of genetic testing, the FDA has “approved an imaging scan called the DaTscan. This technique allows doctors to see detailed pictures of the brain’s dopamine system.” Furthermore, “The results of a DaTscan can’t show that you have Parkinson’s, but they can help your doctor confirm a diagnosis or rule out a Parkinson’s mimic”(3).
Ethical Considerations:
There is always a concern for privacy when it comes to genetic testing. Our genes contain personal biological information, so it is recommended that one doesn’t get tested if (1) it’s not needed or (2) doesn’t live in a nation-state where genetic privacy rights are strongly protected. It is important that you weigh the pro and cons of getting testing especially if the testing could benefit treatment management.
Potential downsides of getting the test include (1) getting results that are not conclusive, (2) increased stress or anxiety from seeing results, and (3) getting misdiagnosed or misinformed. According to Roy Alcalay(1), an assistant professor of neurology at the Taub Institute, “positive findings may induce anxiety among first degree family members (who have a 50% chance of carrying the genetic risk as well), and a fear of discrimination (e.g. for employment or insurance purposes) based on the genetic findings”(1).
Asking the Right Questions Before Getting the Test:
Given the large variability of inheritance, the chances that a child, nephew, or aunt will test positive is largely incalculable. Generally, it would be advantageous for one to determine if the disease is either autosomal dominant or autosomal recessive. However, this method of calculating the probability is not effective because “pedigrees rarely follow that aforementioned well-defined Mendelian inheritance patterns”(4).
Testing positive or negative is often misleading for PD. Oftentimes patients will test positive for PD and either not have or have another disease. For patients with a family history of PD, however, testing positive for PD is an indication that the patient should see a specialist and seek a guided treatment managed with consideration of the additional information from the genetic test. For patients who tested under these similar familial circumstances, but instead tested negatively, it is important that they continue to be aware of their familial risk factors and seek additional information as it becomes available.
If you get a test and would like to share the results with a doctor, it is important that you forward the information effectively. That is to inform your doctor why you got the test and what concerns you had leading up. Discuss with your doctor if there are any recommend steps or additional informative outlets about your test results.
For those who test positive, an additional DaTscan which has been approved by the FDA is recommended so that doctors can collect additional information on the dopaminergic neurons (3). While a positive test does not determine Parkinson’s disease conclusively, it is important that a patient tries to decrease other risk factors associated with the environment. “Exposure to certain toxins or environmental factors may increase the risk of later Parkinson’s disease, but the risk is relatively small”(7). In other words, it is encouraged to avoid toxins, but the effect is small compared to other risk factors that are already at play.
Works Cited
(1) Alcalay, R. N. (2016, April 15). Parkinson’s: risk factors, genetic testing and therapies. Retrieved from http://blogs.biomedcentral.com/on-medicine/2016/04/18/parkinsons-risk-factors-genetic-testing-therapies/.
(2) EurekAlertAAAS. (2007, February 22). Low-cost Parkinson’s disease diagnostic test a world first. Retrieved from https://www.eurekalert.org/pub_releases/2007-02/ra-lpd022207.php.
(3) How Parkinson’s Disease Is Diagnosed. (n.d.). Retrieved from https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/how-parkinson-disease-is-diagnosed.
(4) Klein, C., & Westenberger, A. (2012, January). Genetics of Parkinson’s disease. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3253033/.
(5) Parkinson disease – Genetics Home Reference – NIH. (n.d.). Retrieved from https://ghr.nlm.nih.gov/condition/parkinson-disease#resources.
(6) Parkinson’s disease. (n.d.). Retrieved from https://www.snpedia.com/index.php/Parkinson’s_disease.
(7) Parkinson’s disease. (2018, June 30). Retrieved from https://www.mayoclinic.org/diseases-conditions/parkinsons-disease/symptoms-causes/syc-20376055.
(8) Parkinson’s Disease: Symptoms, Causes, and Treatment. (n.d.). Retrieved from https://www.webmd.com/parkinsons-disease/ss/slideshow-parkinsons-overview.
