By Marianne Lamarche
This year, an estimated 74,200 people in the United States will be diagnosed with non-Hodgkin Lymphoma, the seventh most common cancer in both men and women. With an overall five-year survival rate of only 71%, this cancer poses a devastating threat to the health of thousands every year. As genetic testing technology flourishes, however, scientific advances are providing hope for lymphoma and other similar diseases. Here is everything you need to know about the groundbreaking technology and what it means for you and your family.
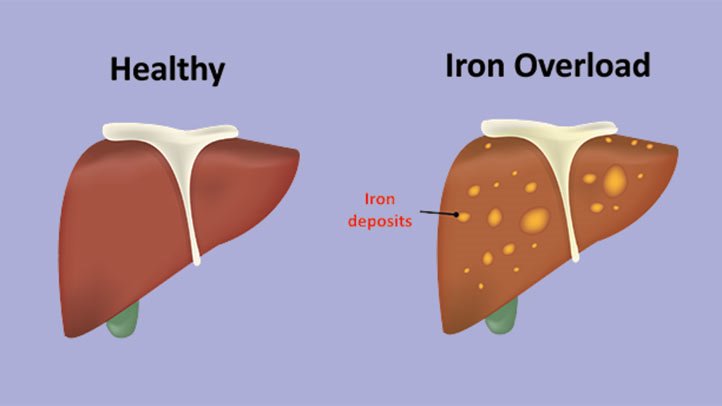
A 2006 study by the National Cancer Institute found that SNPs in two genes, tumor necrosis factor-alpha and lymphotoxin-alpha, were associated with a 1.31x increase in non-Hodgkin lymphoma. These genes affect inflammatory and innate immune responses, which can result in patients with lymphoma struggling to fight off infections. This could make the patients disastrously sick, so doctors searched far and wide for a way to detect these genes as early as possible.
Recently, the Mayo Clinic became the first in the US to offer genetic testing for Lymphoma. While the clinic did not describe exactly what type of test this entails or how much it would cost, the director of the Center for Individualized Medicine at the Mayo Clinic has stated its appeal. “Diagnostic tests such as the Lymph2Cx test will address an unmet need of cancer patients in the U.S. and worldwide,” Dr. Stewart said. “New tests like this help us identify accurate diagnoses and treatments quickly, saving time and money, and, ultimately, transforming patient care.” By studying gene expression and mutations, doctors may be able to more clearly define which patients will respond best to certain therapies, potentially allowing them to treat patients without intrusive chemotherapy.
But we have to consider that these new discoveries still have some limitations. The research on the proinflammatory cytokosine genes listed above was associated with a marked increase in non-Hodgkin lymphoma, but other variations that impact the trait might remain unknown. In general, more research needs to be conducted, as the researchers themselves stated that their “results require replication”. Due to the relatively new nature of these studies, genetic testing might not be the best idea for everyone, since there is so much left to learn about these genes and their impacts on non-Hodgkin lymphoma, and the results of the testing could be misleading.
Results of genetic testing for non-Hodgkin lymphoma could also have some adverse ethical consequences. Dr. Staudt, the lead author of a 2018 study from the New England Journal of Medicine, believes that lymphoma patients should discuss the pros and cons of genetic testing with their oncologist. As cancer research is still in developmental stages, there may not be drugs available for every mutation found in lymphoma patients. In this scenario, their best option for treatment could still be chemotherapy. However, for patients not yet diagnosed with lymphoma but who fear they might be susceptible to it in the future, genetic testing could help them discover if they possess the genes that are associated with an increased risk for non-Hodgkin lymphoma. This also has ethical considerations, though, because if they find out they possess the gene, they might develop chronic stress and experience a decline in their quality of life, whereas even if they discover they don’t possess it, there are so many other branches of lymphoma that they might still become sick despite their efforts to be proactive.
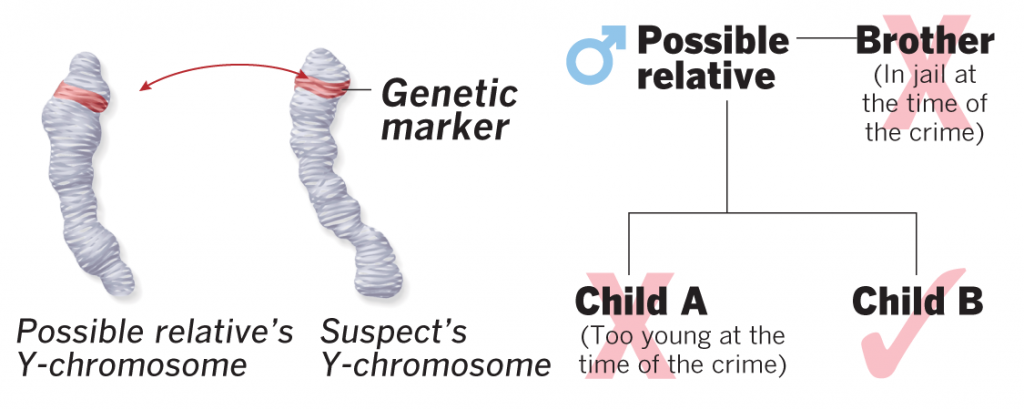
Family history does not have a strong impact on the likelihood of contracting lymphoma; it isn’t currently found to run in families, although your risk might be slightly increased if a first-degree relative has had lymphoma.Thus, you may want to get this genetic test if a parent or sibling has had lymphoma in the past. If you do test positive, however, there are a few lymphoma risk factors that you should avoid to decrease your chances of becoming ill. Medical conditions or treatments that weaken the immune system, such as HIV or post-organ transplant medicine, autoimmune conditions, the Epstein-Barr virus, a Helicobacter pylori infection, having received chemotherapy or radiation for another cancer, or having celiac disease are all associated with an increased risk of developing the condition. But because most of these factors aren’t under your control, the most important reaction to a positive test would be to see an oncologist frequently to detect lymphomatic cells ASAP.
Genetic testing for diseases is a new, potentially life-changing field, but it must continue to develop in order to fully help as many people as possible without infringing on medical and personal privacy and rights. In the case of lymphoma, it is encouraging that new tests may be able to identify the best and most effective treatments for patients, although the lack of control over developing the disease reduces the impact of proactive genetic knowledge. There is still much work to be done – but thankfully, researchers are on the right track towards a healthier, brighter future for you and everyone you care about. Make sure to keep visiting your doctors regularly, maintain a healthy lifestyle, and stay up-to-date on new medical options available. These steps will help to ensure the best outcome possible for your health and wellbeing!
References
Causes: Non-Hodgkin Lymphoma. (2018, October 19). Retrieved from https://www.nhs.uk/conditions/non-hodgkin-lymphoma/causes/.
Katus, S., Roan, S., Raeburn, P., Steele, M. F., & Takeda, A. (2018, April 20). Genetic Testing Reveals Many Different Types of Lymphoma. Retrieved from https://www.everydayhealth.com/lymphoma/treatment/genetic-testing-reveals-many-different-types-lymphoma/.
Lymphoma – Non-Hodgkin – Statistics. (2019, February 28). Retrieved from https://www.cancer.net/cancer-types/lymphoma-non-hodgkin/statistics.
Lymphoma. (2009, December 1). Retrieved from https://www.snpedia.com/index.php/Lymphoma.
Mayo Clinic first in U.S. to offer genetic test for lymphoma. (2019, May 30). Retrieved from https://www.mayo.edu/research/forefront/mayo-clinic-first-us-offer-genetic-test-lymphoma.
Wang, S. S., Cerhan, J. R., Hartge, P., Davis, S., Cozen, W., Severson, R. K., … Rothman, N. (2006). Common Genetic Variants in Proinflammatory and Other Immunoregulatory Genes and Risk for Non-Hodgkin Lymphoma. Cancer Research, 66(19), 9771–9780. doi: 10.1158/0008-5472.can-06-0324