Clinical Decision Support System: Evaluation of Physician Behavior Responses to Implementation in Three Cardiac Settings in Boston, MA
Table 1. Summary of Current Interventions:
| Author & Year | Intervention Setting, Description, and Comparison Group(s) | Study Population Description and Sample Size | Effect Measure (Variables) | Results including Test Statistics and Significance | Follow-up Time |
| FY Lin (2013) (LINK) | The success of a criteria decision support tool (AUC-DST) on increasing the correct choice of clinical tests and decisions was evaluated. A multicenter cohort study was conducted tracking physician decisions for imaging of patients with suspected coronary artery disease. | Tests ordered by 100 physicians fitting the criteria of employment within 1 of 3 chosen single-specialty cardiology practices were tracked. 472 patients age 56 +/- 9.6 years were selected as study group. 52% had prior CAD. | 3 specific cardiac imaging tests were evaluated: MPS (myocardial perfusion scintigraphy), STE (stress echocardiography), and CCTA (coronary computed tomographic angiography). Appropriateness of each test was assessed and tests were found to fall in one of 4 categories: Appropriate, Uncertain, Inappropriate, or Not Addressed.
|
Over the 8 month study period the percent of test usage were found to be: MPS (72%), STE (24%), CCTA (5%). Appropriateness of tests in the first 2 months with the last 2 months showed an increase in appropriate tests from 22% to 6% (p<0.001). Intended medical therapy changes increased from 11% to 32% (p=0.001). | Clinical decisions for imaging orders were evaluated throughout an 8 month period with an emphasis on the first 2 months and the last 2 months of decision tool intervention. |
|
Beeckman, et al (2012) (LINK)
|
The study was done in 4 nursing homes in Belgium to assess whether a CDSS could help decrease the rate of pressure ulcers in the elderly inhabitants. Nursing homes which had the CDSS were compared against similar nursing homes without the CDSS. The experimental arm was involved in a multi-faceted tailored implementation intervention of a clinical decision support system, including interactive education, reminders, monitoring, feedback and leadership. The control arm received a hard-copy of the pressure ulcer prevention protocol, supported by standardized 30 min group lecture. |
Random sample of 11 wards (6 experimental; 5 control) in a convenience sample of 4 nursing homes in Belgium. In total, 464 nursing home residents and 118 healthcare professionals participated. | The primary outcome measures were the ward level proportion of residents at risk receiving fully adequate prevention measures and the ward level proportion of residents at risk receiving no adequate prevention measures respectively. | Patients in the intervention arm were significantly more likely to receive fully adequate pressure ulcer prevention when seated in a chair (F = 16.4, P = 0.003). No significant improvement was observed on pressure ulcer prevalence and knowledge of the professionals. While baseline attitude scores were comparable between both groups [exp. 74.3% vs. contr. 74.5% (P = 0.92)], the mean score after the intervention was 83.5% in the experimental group vs. 72.1% in the control group (F = 15.12, P < 0.001). | A followup observation for retention of knowledge by the nursing home staff was not conducted; it was proposed as something to do in the future in the discussion section. |
| JE Tisdale (2014) (LINK)
|
Study was conducted in an academic medical center located in an urban area. 2400 patients who had been admitted for cardiac care were evaluated. Electronic medical records were used to create a risk score for QTc prolongation to use in the CDSS to attempt to reduce negative outcomes through clinical efforts. The comparison was done internally. | Patients with a moderate or high risk of QTc prolongation were the focus of the study. Drugs prescribed associated with torsades de pointes were of concern. Patient assessments were divided into before and after CDSS use (n=1200 for each). | QTc interval prolongation was defined as >500ms or an increase of >=60ms from baseline. If patients had >500ms prolongation they were assessed just on the increase. | CDSS use for the study was independently associated with reduction of QTc prolongation risks (OR=0.65, 95% conf. interval 0.56-0.89, p<0.0001). CDSS use reduced use of non-cardiac drugs recognized to cause torsades de pointes (OR=0.79, 95% conf interval 0.63 – 0.91, p=0.03). | No follow up was done. Study concluded after end points were assessed from initial CDSS implementation. |
Community Guide Update and Rationale for Intervention:
The strategy to use CDSS to improve clinical care for cardiac disease and strengthen prevention of CVD is strongly recommended. It is strongly recommended that physicians caring for CVD patients should implement a CDSS into their clinical practice to improve the identification of risk factors, ordering of tests, and providing better overall care.
A strong recommendation for CDSS use for prevention and care of CVD in clinical settings can be made on the basis of improved accuracy, better decision making, and decreased redundancy in practice. Lin et al demonstrated that CDSS use can increase the rate of correct test ordering by physicians (2013). Thus, providing evidence a computerized system to organize clinical information improves physician test decisions in cardiac patients. Tisdale et al. showed strong correlations between CDSS use and improved decision making in pharmaceutical use in at risk patients for QTc prolongation, presenting compelling evidence of the ability of CDSS to alter behavior (2014). CDSS systems have proven to be of great benefit to the structuring of physician clinical behavior and increase patient safety (Friedlin 2007). Cardiovascular disease presents significant clinical challenges and interventions in healthcare delivery systems have been suggested for the promotion of health in this area (Fuster 2011). Ultimately CDSS is a recommended tool for standardizing physician behavior and improving patient care. It is the goal for practitioners to quickly and accurately review patient histories and make collaborative decisions using computerized support systems in the formation of useful cardiac disease treatment and prevention strategies. Theoretical Framework/Model:
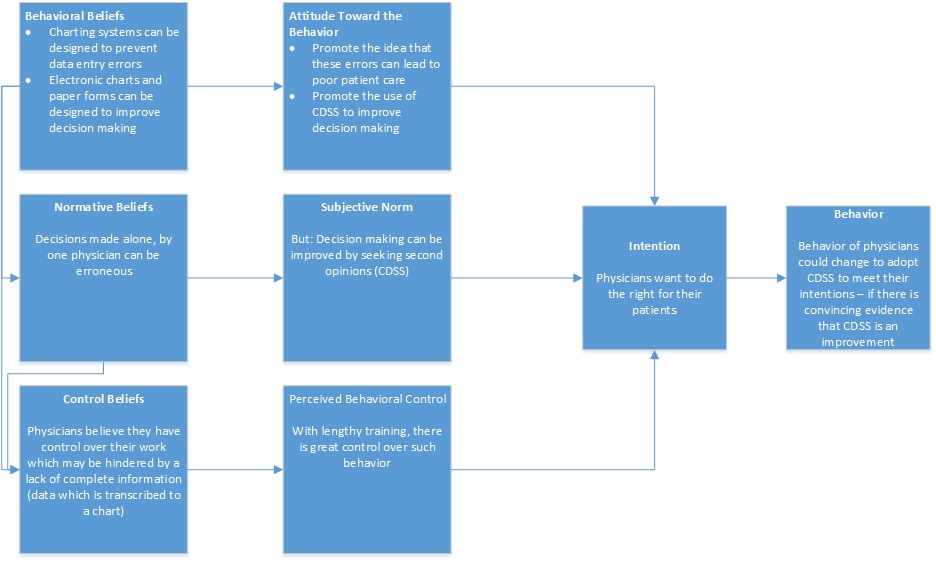
We have chosen to utilize the Theory of Planned Behavior (TPB) in planning an intervention program to assist physicians in their decision making process. The theory of planned behavior was proposed by Icek Azjen in 1985, and it links beliefs and actual behavior. The theory has also been suggested to be useful in the study of healthcare provider behavior (Millstein 1996).
Constructs:
In the context of this theory, there are three beliefs which are considered: behavioral, normative, and control beliefs. These beliefs lead to attitudes toward behavior, subjective norms, and perceived behavioral control, respectively. These then lead to intent and behavior.
Behavioral Beliefs: Behavioral beliefs are defined as an individual’s belief on the consequences of their behavior. It is based on a probability that doing something will lead to an intended outcome–in this case, making proper or good decisions will lead to proper or good patient care..
Normative Beliefs: Normative beliefs are an individual’s perception of the conventions for how to act in a given situation. In this case, it is how a physician believes most other physicians would make decisions in a patient-care scenario. The CDSS is meant to intervene and steer a physician toward a gold-standard of normative belief (what does the literature say?) rather than what the physician’s perceived norms are. Subjective norms are norms which are influenced by the judgement of significant persons such as co-workers or leading authorities.
Control Beliefs: Control beliefs are an individual’s beleifs about factors which might hinder or help their actions and performance. Percieved behavioral control is the individual’s perception of what might help or hinder their performance. In our intervention perceived behavioral control is the major focus as we aim to alter the control physicians perceive in non-computerized charting. CDSS serves as a tool which positively alters the control beliefs and perceived behavioral control of physicians. The tool is to reduce hindrances and assist standardizing actions in accordance with training. Intention is an individual’s beliefs and readiness to perform a given behavior. The behavior is the final observable action after intention has been made. (Azjen, 1985; “Theory of Planned Behavior”, Azjen, 2016)
Diagram of Conceptual Model:
Target Population:
The target population for the CDSS program are cardiac specialist physicians in large hospital settings with specialized CVD departments. Specifically, three hospitals in Boston have been selected to take part in the study. Cardiac floors in Bringham and Woman’s Hospital, Massachusetts General Hospital, and Beth Israel Deaconess Medical Center have been selected as study sites. Cardiac physicians of interest care for patients with risk factors for developing CVD and also care for patients who are at risk for worsening their CVD conditions. Although health disparities may exist among patients with CVD it is not the focus of the study, as we will focus on the intervention of CDSS and the subsequent alteration of physician behavior.
Logic Model, Causal and Intervention Hypotheses, and Intervention Strategies:
Table 2: Intervention Method and Strategies
| Intervention Method | Alignment with Theory | Intervention Strategy |
| Prevent errors in physician clinical data entry. | The concept of behavioral control in the theory of planned behavior frames the intervention for reducing errors. Reducing errors is accomplished by making the intention and finally behavior of physicians more accurate. Perceived behavioral control is altered by documentation forms and templates. Physicians are forced to follow templates and concede some freedom of input so that the CDSS sorts information that is to be recorded. | Create documentation forms and templates that structure the clinical identification of risks and prompt prevention of CVD. Prevents omission and comission errors by displaying options on screen to populate data fields, and requiring data be entered in order and take a standard form. |
| Increase physician access to relevant patient data in dealing with CVD at-risk patients. | The behavioral control concept of the theory aligns with increased access. Behavioral beliefs of physicians are positively reinforced by access to relevant data and intention to act is strengthened leading to better clinical decisions. Physicians are able to make a strongly intended behavior that leads to better clinical actions. | Present relevant patient data for patients at risk for CVD. Make the data presentation so that physicians can see the full patient profile easily and in a simple format. Combines data to create a complete clinical framework for each patient. Optimization of decision making by providing clear and concise information otherwise difficult or overly complex to analyze. |
| Expand physician ability to access a complete clinical patient history. | The concept of normative beliefs leading to intention and thus affecting behavior is key to the success of CDSS. Providing a complete history reduces possible errors in judgement based on a physician’s normative beliefs about patient histories and subsequent risks for CVD. Altering the adherence to normative beliefs about patients serves to allow more objectivity in clinical decision making. | Creation of protocol pathways that extend over time to create an environment of clinical continuity. CDSS based timelines allow physicians to see full history and accurately assess CVD risk. Give structure to decision making process. Suggestions can be made by the CDSS to indicate best practice given the patient variables. |
| Promote in physicians the quick recognition of real-time clinical needs. | Intervening between behavioral control and intention promotes better clinical decision making. Perceived behavioral control is increased by the CDSS and the physicians trust in the system. In situations where the lack of timely information would normally cause the physician to have a sense of control not based on accurate information, the CDSS ensures intention of clinical decision behavior is based on up to date information. | Alerts and reminders are used to immediately notify physicians of new test results or CVD risk factors recorded by other members of the clinical team. Important alerts indicate when possible errors have occurred or when new information has been uploaded that changes information for clinical decisions. |
Table 3: Program Logic Model of Intervention
| Inputs/Resources | Activities | Outputs | Short-term Outcomes | Intermediate Outcomes | Long-term Outcomes |
| 1. Study grant funds are allocated for the development of electronic forms with partial funding and input from each hospital. Hospital personnel are needed to tailor forms to clinical practice protocols specific for each hospital. Hospital staff is needed to assist in the training of physicians. | New documentation forms are created to be used for clinical charting.These new documentation forms have a well-thought out template for use by physicians in taking care of potential and actual CVD patients. These documentation forms are designed to quickly allow a physician to go through all the necessary things in the care of such patients by using a checklist format. | Electronic checklist forms are generated for every patient. Cardiac checklists are designed to be used in alignment with the standard operating procedures of each hospital as designated by clinical administrators. | The behavior of physician for clinical charting would change. Physicians would be able to write their observations and test orders on a standardized documentation form, instead of an older method such as writing orders freely. | Omission error events when managing a patient case should decrease from baseline counts of such events from the paper system. | Physician behavior to comply with standard forms will continue and reduce overall errors. Because omission error events are reduced, the health of patients should also improve because their cases are managed more ideally. Decreases in CVD morbidity should be a long-term advantage. |
| 2. Funds to purchase study CDSS software packages to integrate patient history with other forms is allocated. Hospitals allocate personnel (nurses and medical techs) to input patient profiles as admissions occur. Hospital staff is needed to assist in the training of physicians. |
Presentation of relevant patient data in an integrated way that is easily accessible and updated. Make the data presentation so that physicians can see the patient profile easily and in a simple format. Combines data to create a complete clinical framework for each patient. Optimization of decision making by providing clear and concise information otherwise difficult or overly complex to analyze. |
These changes would be on every electronic charting computer, a trial license would be used for the study duration. Each cardiac floor could allocate additional resources at their discretion given their current computer systems. |
Decisions could be made in an easier fashion if data is accessible cleanly and clearly with integration in mind. This aligns with the behavioral control beliefs which are altered by submission of control to the CDSS instead of completely relying on traditional possibly poorly integrated methods.
|
Physicians can make decisions with all necessary information. Communication between physicians and others may also change. This is especially useful when attending cardiac specialists must transfer care of patients to other specialists or team practitioners.
Decisions could also be made with a higher degree of certainty if there is a second opinion of the gold standard case management of the current patient. |
Physician behavior to rely on clinical integration software will improve standardization of care. Patients will benefit from a greater continuity of care and consistency from all providers using the CDSS. Continuity and consistency lead to better decisions and improved health outcomes leading to decreased morbidity. |
| 3. Study grant funds are allocated to purchase software packages to provide patient history forms and registries. Hospital staff is needed to input patient histories and maintain continuous histories as medical records are transferred and updated. Hospital staff is needed to assist in the training of physicians. |
Creation of protocol pathways that extend over time to create an environment of clinical continuity. CDSS based timelines allow physicians to see full history and accurately assess CVD risk. Give structure to decision making process. Suggestions can be made by the CDSS to indicate best practice given the patient variables. |
Patient history software would be on every electronic charting computer used in the intervention for the trial period and then could be renewed for the future depending on study results.
|
Altering the normative beliefs of the physician allows for improved decision making. For example a physician may believe he or she has a complete view of the patient even though much information has been overlooked. Providing a complete history in an easily accessible manner would enable physicians to potentially reduce errors in judgement and oversight. | Reducing errors of judgement would improve the care of patients during their stay in the hospital. | Physicians overtime would rely on the CDSS to provide accurate and long-term patient data. Patients could see an improved outcomes due to decisions being made in a more informed manner. |
| 4. Study grant funds will be allocated to purchase alert software packages that integrate with the charts and medical history software for the CDSS. Hospital staff is needed to assist in the training of physicians. | A real-time alerts system would be implemented for computerized charting activities. Alerts and reminders are used to immediately notify physicians of new test results or CVD risk factors recorded by other members of the clinical team. Important alerts indicate when possible errors have occurred or when new information has been uploaded that changes information for clinical decisions. | These changes would be on every electronic charting computer, the study grant would purchase a trial license to have this add-on software and hospitals would be responsible for purchasing any other subscriptions for future use. | Physician’s behavior should change in accordance with the alerts or reminders. Real-time updates act as an intervention between the physicians behavioral beliefs and intention. system. Computerized updates that pop-up on screen are designed to be difficult to ignore and require a response when reviewing electronic charts. | Physicians can make decisions with all necessary information quickly and easily when alerts are presented. Communication between physicians and others may also change (obtaining information directly from a chart, easily, rather than calling someone else) increasing the speed at which decisions can be made.
Errors related to delayed care would be reduced in patients. For example, an alert could remind physicians of a new test result that might alter the course of treatment, that might have otherwise been delayed without the alert system. |
Physicians are made more aware of real-time patient conditions leading to improved clinical behavior. Patients should see an improved outcome during their stay due to decisions being made in a more informed manner. Things such as medications being given according to a lab test result could happen in a more streamlined manner. Ultimately decreasing morbidity and in cases where mistakes could be fatal it would decrease mortality. |
Intervention Hypotheses:
- Documentation forms and templates will lead to decreases in physician errors for clinical data input.
- Presentation of relevant patient data will improve physician knowledge of the greater clinical patient status and improve decision making.
- Protocol pathways to produce clinical continuity will improve physician assessment of CVD risks.
- Alerts and reminders will decrease errors in clinical decision making and improve patient care.
Causal Hypotheses:
- Decreases in physician data errors will lead to a decrease in accidental treatments and inaccurate classification of CVD risk.
- Increased knowledge of patient status and improved clinical decision making will lead to reduced prevalence of CVD in patient population.
- Improved physician assessment of CVD risk factors will decrease overall patient morbidity of CVD.
- Improved patient care (from alerts and reminders) will reduce prevalence and/or worsening of CVD disease states and decrease mortality from wrongful treatment.
SMART Objectives:
Goal 1: Decrease input errors during chart documentation by physicians.
- Objective 1: At the end of our 1 year evaluation period, documentation errors such as typos, and omissions will be reduced by 50% or greater to indicate success of CDSS implementation.
Goal 2: Improved presentation of patient data will improve decision making and clinical case management by physicians.
- Objective 1: Overall rate of patients receiving time-sensitive medicine orders from doctors when required (based on vital signs and nurse notes) will increase by 20% or more than before the intervention by 3 months and be maintained or exceeded for the full study.
Goal 3: Improved data presentation will improve CVD risk factor case management.
- Objective 1: Patients who present with potential CVD symptoms will be assigned as being a CVD or non-CVD patient with 95% certainty given standardized CVD risk metrics as designated by the hospital clinical administrators after 3 months time.
- Objective 2: At 6 months, and 1 year, following the intervention this measure should continue to be 95%.
Goal 4: Alerts should improve “catching” of life threatening cardiovascular events before the event.
- Objective 1: EKG’s being done promptly will be the focus of the alerts system. We will not measure actual health states but will ensure that EKGs are done within 10 minutes of whenever a patient is admitted to the floor. This is a preventive measure which has been recommended by the American Heart Association to catch potential life threatening heart conditions such as ST elevation myocardial infarction (AHA, 2016).
Table 4: Stakeholders Roles and Questions:
| Stakeholder | Role in Intervention | Evaluation Questions from Stakeholder | Effect on Stakeholder of a Successful Program | Effect on Stakeholder of an Unsuccessful Program |
| Physicians | Program participants | How will this impact patient care protocols?
Will the CDSS be tested, easy to use and free of bugs? Do CDSS improve patient outcomes?
|
Reduction in accidental treatment orders. Reduction in clinical errors. Increase efficiency and patient load abilities. | Interfere with normal clinical activities. Delay treatments. Confer no clinical advantage and not reduce patient morbidity. |
| Cardiac Patients | Recipient of clinical care | Will CDSS use increase safety?
Will care be delayed or altered during the study? |
Receive accurate and needed care. Benefit from better physician decisions. Reduced chance of treatment error. Reduced chance for developing or worsening CVD symptoms. | Experience delays in care. May not see benefits or reduction in symptoms. |
| Hospital Administrators | Help implement program and ensure integration of software | What are the costs of a CDSS?
Does CDSS implantation lead to a reduction in malpractice? Are reimbursement rates affected by CDSS? |
Increase productivity and profits. Reduce unnecessary use of hospital resources by poorly informed physicians. Reduce morbidity and mortality metrics in the long run and increase hospital rating. | Decrease productivity and increase need for technical troubleshooting. Cost the hospital a considerable amount and not present enough advantages to make it a sound business move. |
| Program Director and Staff | Direct the program and evaluate physicians | How has CDSS success been measured in the past?
Will the timeline for the intervention be sufficient for our purposes? Are evaluation metrics consistent with previous studies on CDSS success? |
Receive results that are favorable for publication. Strengthen hospital partner relationships. Lay foundation for further study in other settings and with longer timelines. Promote use of methods outlined in study. | Possibly damage academic reputation and hospital partnerships. Reduce funding opportunities for future studies. |
Evaluation Design:
The study will utilize a randomized control trial. All patients will receive standard care with the only difference being the physician will have been trained on CDSS use and have access to CDSS software. Patients admitted to the cardiac floors of the study hospitals will be randomized by there medical record numbers, the even numbers will be grouped as the control arm and sent to beds under charge of physicians not using CDSS. The odd numbered patients will be placed in beds under charge of physicians using the CDSS intervention. Each of the three intervention groups will be matched with the respective control group within each selected hospital as (listed in item 6). Three cardiac floors are the target of the study and have been selected because they are the top care facilities in Boston area for CVD. Physicians in the intervention group will be evaluated on their adherence to the CDSS prompts and responses. Chart audits will be conducted to see if CDSS prompts were followed in the intervention group and if mistakes were corrected. In the control group charts will be audited for mistakes. Intervention and control groups will also be compared for patient outcome metrics and to see if CDSS may have had a positive effect. R O1 X O2 O3 (Intervention Group A) R O1 O2 O3 (Control Group A) R O1 X O2 O3 (Intervention Group B) R O1 O2 O3 (Control Group B) R O1 X O2 O3 (Intervention Group C) R O1 O2 O3 (Control Group C) (O1 = initial chart input, O2 = first chart audit, O3 = second chart audit)
Threats to Internal Validity: Internal threats are minimized by the randomization and use of matched control groups. However, possible threats to internal validity remain such as patient mortality, dropout, and regression to the mean given the possibility of receiving a high number of very ill patients. Given the large projected sample size it is anticipated that little internal validity will be threatened.
- Drop Out: Physicians may dropout of the study due to illness or random needs. This could skew the ability to test if physician chart adherence and patient outcomes are due to CDSS use.
- Maturation: It is possible that patients may have reductions in severity or prevalence of symptoms not due to the CDSS intervention. Even with matched control groups it is still possible for maturation to skew the evaluation of intervention results, but given the large sample size and randomization the chance is lessened as much as possible.
- Regression to the mean: It is possible that most of the CVD patients may be of very ill health upon admittance and thus can skew the results. Patients being admitted and who remain for the entire study may be of poorer health regardless of receiving intervention or not. Improvements recorded may not be attributable to the intervention in this scenario.
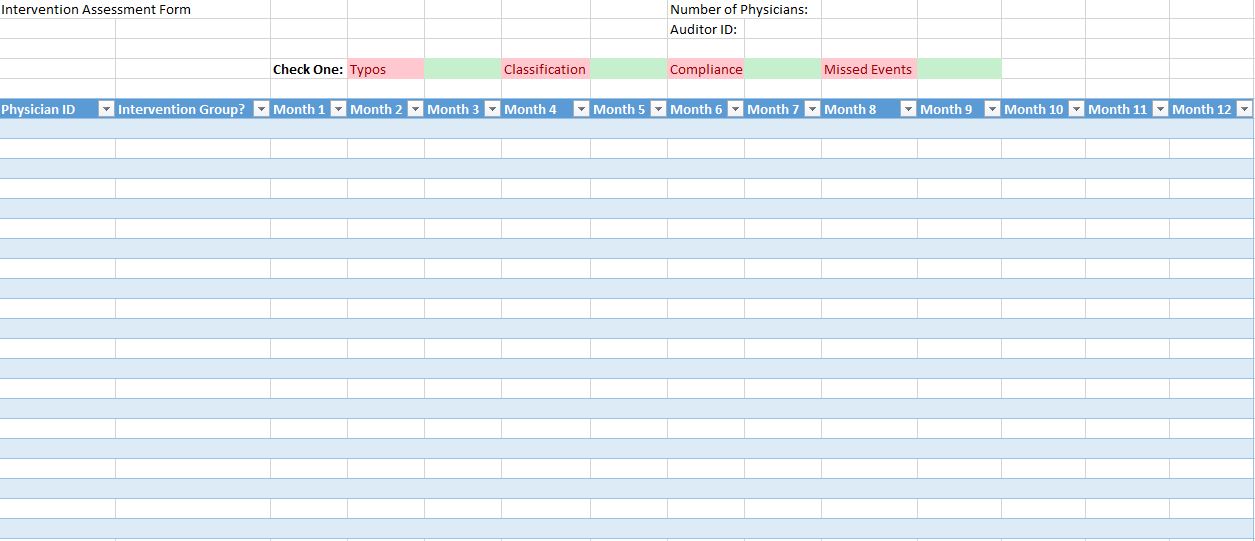
Table 5: Summary of Measures
| Short-term or Intermediate Outcome Variable | Scale, Questionnaire, Assessment Method | Brief Description of Instrument | Example item (for surveys, scales, or questionnaires) | Reliability and/or Validity Description |
| Accuracy in Charting | The accuracy of charting (reduction of omissions, and typos) will be evaluated by chart review or auditing. | Chart auditing is a well-known method for assessing accuracy of charting. The instrument used by reviewers to audit the areas of interest in an electronic chart will be based on a chart audit strategies guide which was published in 2009 for assessing nursing documentation by Frankie WH Wong. | Scale:
For a random patient: How many typos are there in the chart from X to Y dates? (X and Y being dates that a patient was in the hospital, during the time the software was being used.) |
A 2009 study which employed auditing of nurse’s charts found that inter-rater reliablity exceeded 95% (Weinberger, 1995). Another study which reported an inter-rater reliability of 75% for chart-keeping in auditing family physician’s charts (Goulet et al, 2007). Both studies insinuate or claim that as long as auditors are trained, this method is accurately estimates what is being measured. |
| Physician Chart Usage | We will measure the length of time and number of times that a chart is opened by the physician. | Length of time a chart is opened will be recorded by software, which will also log who opened the chart. The number of times a chart is opened will also be kept track of by the software and an auditor will fill in a form (see below for the form) to keep track of number of times a chart was opened. | Questionnaire: How many times was the chart opened by physician X (where X is the physician being studied)? | Please see above for the reliability of an auditor. A study by Schultz et al, conducted in 2013 demonstrated that data from EHR software is reliable. |
| Improved Compliance with Cardiac Quality Measures by Physicians | The assessment of effectiveness will be done by obtaining a rate of compliance. Compliance is a binary outcome of best practice in writing orders or being not compliant. | The instrument is a CDSS checklist that helps with the management of cardiac patients. | Example questionnaire item for auditor:
How long has it been since the patient was admitted? Is it appropriate to prescribe antibiotics at this time? |
Such a CDSS has been studied in resident doctors and a paper was published in 2008 which details the effectiveness of such a method and measure (Riggio et al, 2008). |
| Missed Events | The implementation of real-time reminders should decrease missed events. These will be evaluated by looking at the electronic chart and searching for events where a lab was ordered but not done on time. | The instrument is an auditing checklist similar to that used in a 2009 study which assessed the use of electronic health-record based alerts for influenza vaccination in children (Fiks et al, 2009). | Example item (scale): Was an EKG conducted within 10 minutes of admission? | Please see measure one for the reliability of auditors being used to assess a measure such as this. |
Process Evaluation and Data Collection Forms:
Recruitment and enrollment:
Recruitment and enrollment will first begin by consulting the leadership at the hospital which is responsible for representing the physicians who work in the hospital. After receiving approval we will directly ask the cardiac physicians to participate in our study, via email, and in person, to join our study which aims to compare patient care between CDSS use and non-use. Patients cared by selected physicians will have a informed consent letter signed prior to admittance. The hospital leadership will also be prompted to encourage physicians to join and incentives such as gift cards to encourage physicians to join if adequate enrollment is not observed during the initial recruitment phase.
Sample letter sent to hospital administration to enroll in study:
Dear Hospital Administration,
We have selected your hospital to showcase and evaluate the success of a Clinical Decision Support System (CDSS) for cardiac patients. You have been selected for your outstanding performance in cardiac disease treatment and will be part of a three hospital clinical trial to evaluate the utility of the CDSS on improving patient outcomes through better clinical decision making by physicians. We feel that the evaluation of the CDSS will help your hospital improve in many metrics and will give data usable for you to decide what CDSS implementation will work for you in the future.
The pilot study will take place over the next year and will require minimal expenses from you as we have secured grant partnerships. Please let us know if you would be interested in participating. We hope you will join us on this journey to improving patient care and increasing physician productivity.
Sincerly,
CDSS Research Group
Sample letter which administration would send to the physicians:
Dear Dr _____
We are currently evaluating a new clinical decision support system designed by Company X. The system will enhance our current charting software to assist you in patient care. The add-ons will now provide reminders for time-sensitive lab orders. The system will also improve the manner in which data is presented to you, making the patient history and vital signs reporting more standardized. The add-ons also include paper forms with checklists to assist you in referencing our protocols for caring for cardiac patients.
We will be evaluating this software for the next year as we are looking for new methods to improve our patient care objectives. This new software intervention is aimed at reducing stress in making decisions and helping you to consider everything in your patient care duties.
Please let us know if you have any concerns or questions with this new system.
Sincerely,
Clinical Administrator _____________________
Hospital _______________________
Sample Assessment form for Auditors:
Attrition:
We plan to acquire information from various sources: the floor managers, charge nurses, the actual physicians, as well as the actual data. The majority of our intervention would be assessed through data collection from the software/tools and metrics would be easily accessed to compare with non-CDSS charting of control physicians.
References
-
Lin, F. Y., Dunning, A. M., Narula, J., Shaw, L. J., Gransar, H., Berman, D. S., & Min, J. K. (2013). Impact of an automated multimodality point-of-order decision support tool on rates of appropriate testing and clinical decision making for individuals with suspected coronary artery disease: a prospective multicenter study. Journal of the American College of Cardiology, 62(4), 308-316.
-
Beeckman, D., Clays, E., Van Hecke, A., Vanderwee, K., Schoonhoven, L., & Verhaeghe, S. (2013). A multi-faceted tailored strategy to implement an electronic clinical decision support system for pressure ulcer prevention in nursing homes: a two-armed randomized controlled trial. International journal of nursing studies, 50(4), 475-486.
-
Tisdale, J. E., Jaynes, H. A., Kingery, J. R., Overholser, B. R., Mourad, N. A., Trujillo, T. N., & Kovacs, R. J. (2014). Effectiveness of a clinical decision support system for reducing the risk of QT interval prolongation in hospitalized patients. Circulation: Cardiovascular Quality and Outcomes, 7(3), 381-390.
-
Ajzen, I. (1985). From intentions to actions: A theory of planned behavior (pp. 11-39). Springer Berlin Heidelberg.
- Azjen, I. (n.d.). Theory of Planned Behavior. Retrieved June 07, 2016, from http://people.umass.edu/aizen/tpb.html
-
Armitage, C. J., & Conner, M. (2001). Efficacy of the theory of planned behaviour: A meta‐analytic review. British journal of social psychology, 40(4), 471-499.
- http://www.heart.org/HEARTORG/HealthcareResearch/MissionLifelineHomePage/EMS/Recommendations-for-Criteria-for-STEMI-Systems-of-Care_UCM_312070_Article.jsp
-
Riggio, J. M., Sorokin, R., Moxey, E. D., Mather, P., Gould, S., & Kane, G. C. (2009). Effectiveness of a clinical-decision-support system in improving compliance with cardiac-care quality measures and supporting resident training. Academic medicine, 84(12), 1719-1726.
- Friedlin, J., Dexter, P. R., & Overhage, J. M. (2007). Details of a Successful Clinical Decision Support System. AMIA Annual Symposium Proceedings,2007, 254–258.
- Fuster, V., B.B. Kelly, and R. Vedanthan, Global cardiovascular health: urgent need for an intersectoral approach. J Am Coll Cardiol, 2011. 58(12): p. 1208-10.
- Millstein, S.G., Utility of the theories of reasoned action and planned behavior for predicting physician behavior: a prospective analysis. Health Psychol, 1996. 15(5): p. 398-402.
-
Schultz, S. E., Rothwell, D. M., Chen, Z., & Tu, K. (2013). Identifying cases of congestive heart failure from administrative data: a validation study using primary care patient records. Chronic diseases and injuries in Canada, 33(3).
-
Haley, V. B., Van Antwerpen, C., Tserenpuntsag, B., Gase, K. A., Hazamy, P., Doughty, D., … & Stricof, R. L. (2012). Use of administrative data in efficient auditing of hospital-acquired surgical site infections, New York State 2009–2010. Infection Control & Hospital Epidemiology, 33(06), 565-571.
-
Montano, D. E., & Phillips, W. R. (1995). Cancer screening by primary care physicians: a comparison of rates obtained from physician self-report, patient survey, and chart audit. American Journal of Public Health, 85(6), 795-800.
-
Goulet, F., Jacques, A., Gagnon, R., Racette, P., & Sieber, W. (2007). Assessment of Family Physicians’ Performance Using Patient Charts Interrater Reliability and Concordance With Chart-Stimulated Recall Interview. Evaluation & the health professions, 30(4), 376-392.
- Fiks, A. G., Hunter, K. F., Localio, A. R., Grundmeier, R. W., Bryant-Stephens, T., Luberti, A. A., … & Alessandrini, E. A. (2009). Impact of electronic health record-based alerts on influenza vaccination for children with asthma. Pediatrics, 124(1), 159-169.