Group-Based Comprehensive Risk Reduction Intervention Program
Part I. Community Guide Update and Rationale for Intervention
Table 1: Summary of recent intervention
| Author & Year | Intervention Setting, Description, and Comparison Group(s) | Study Population Description and Sample Size | Effect Measure (Variables) | Results including Test Statistics and Significance | Follow-up Time |
| Markham, et al., 2012
|
Design: Three armed, randomized controlled trial of sexual risk avoidance and reduction intervention.
Settings: 15 urban middle schools Intervention: Risk reduction program (RR) and risk avoidance program (RA) were conducted in the study. RR program includes condom skills training and emphasized abstinence. RA program followed abstinence education guideline. Comparison group: receive regular health classes |
1258 middle school students that are predominantly African American and Hispanics
Middle schools are in South Central U.S school district. 78% of the students are from low-income family. |
Delaying sexual initiation, numbers of lifetime sexual partners, unprotected sex | Compare to the control group, the RR program delayed all type of sexual initiation including oral, vaginal or anal sex. OR: 0.65; 95% CI [0.54, 0.77]. Reduction in unprotected sex at last intercourse is also seen in RR program. OR: 0.67; 95% CI [047, 0.96]. RA program delayed sexual initiation among Hispanics. OR: 0.40; 95%CI [0.19. 0.86]. However there is an increased number of recent vaginal sex partners in RA program. OR: 1.69; 95% CI: 1.01, 2.82].
|
4 years (from 2006-2010) |
| DiClemente, et al., 2009 | Design: Randomized controlled trial of a HIV prevention program
Setting: Clinic-based sample in Atlanta, GA. Intervention: 1) Two 4 hour group STD/HIV prevention session 2) provide vouchers to participants to give to their sexual partners to improve accessibility of STD screening or treatment, 3) 4 brief phone calls to follow up and reinforce prevention. Comparison group: 1 hour group session, no further STD/HIV prevention education |
715 African American adolescent female (age 15-21), umarried, not pregnant, sexually active in the past 60 days that seek for sexual health services from 3 clinics in downtown Atl, GA. | Incidence of chlamydial infections and STD/HIV preventative behaviors | Intervention group has reduction of chlamydial infection rate; RR: 0.65; 95% CI [0.42, 0.98].
Higher proportion of consistent condom use is reported. RR: 1.41; 95% CI [1.09, 1.80]. Condom use at last intercourse has also increased in intervention group. RR: 1.30; 95%CI [1.09, 1.54]. |
12 months follow up |
| Morrison-Beedy, et al., 2012 |
Design: Randomized controlled trial of a sexual risk reduction intervention Intervention: 4 weekly 120 minute group sessions and 2 post intervention session. Control group: General health promotion topics |
738 female participants aged 15-19 that are unmarried, not pregnant, sexually active and not given birth within the past 3 months. Majority of the participants are low-income and African American (69%). | Abstinence, number of sexual partners, unprotected sex, total vaginal sex (both protected and unprotected) | Intervention group has a lower rate of vaginal sex at each follow up time (p<0.001).
Intervention reduced the mean frequency of unprotected sex at all follow up months. 8% at 3 months and 9% at 12 months (p<0.05). A higher proportion of participants were abstinent in intervention group than in controls. OR=2.19; 95% CI [1.37, 3.52]. |
3, 6, 12 months follow up |
Community Guide update and rationale for intervention
The community preventive services task force currently recommends group based comprehensive risk reduction targeted towards the adolescents to prevent and reduce teen pregnancy, HIV and other sexually transmitted disease after reviewing 62 studies. The recommendation in 2009 is based on sufficient evidence in self-reported risk behavior, including frequency of any sexual activity, frequency of unprotected sexual activity, and number of sexual partners. However, there is limited directed evidence of effectiveness to reduce teen pregnancy and HIV.
Three studies conducted after the Task Force’s 2009 recommendation were reviewed and found there is sufficient evidence to support group based comprehensive risk reduction intervention. Similar to the results of systematic review, all three studies found frequency of unprotected sex has decreased significantly. Additionally, Frequency of any sexual activity has reduced in the study conducted by Morrison-Beedy, et al. (2012) and Markham, et al. (2012). The Task Force systematic review found significant decrease in number of partners of approximately 14% (OR=0.83, 95% CI 0.74, 0.93). However, there is an increased number of recent vaginal sex partners in RA program in the study conducted by Markham, et al. (2012); OR: 1.69; 95% CI: [1.01, 2.82]. Regardless of the inconsistent findings in number of sexual partners in one study, I recommend group based comprehensive risk reduction program to reduce risky sexual behaviors. There are strong evidence from these studies relating to decrease frequency of unprotected sex and overall sexual activities.
There have been no changes to the recommendation by the Task Force. I would not change the current recommendation status by Task Force. All three studies were effective in promoting protected sex to avoid adverse health outcome. There is no evidence that the intervention should be strongly recommended. The sample size in the three studies are not large enough that it may create some bias. Overall, group based comprehensive risk reduction intervention strategy is effective and should be recommended to promote and reduce risky sexual behaviors among adolescents.
Part II. Theoretical Framework/Model
Theoretical Framework/Model
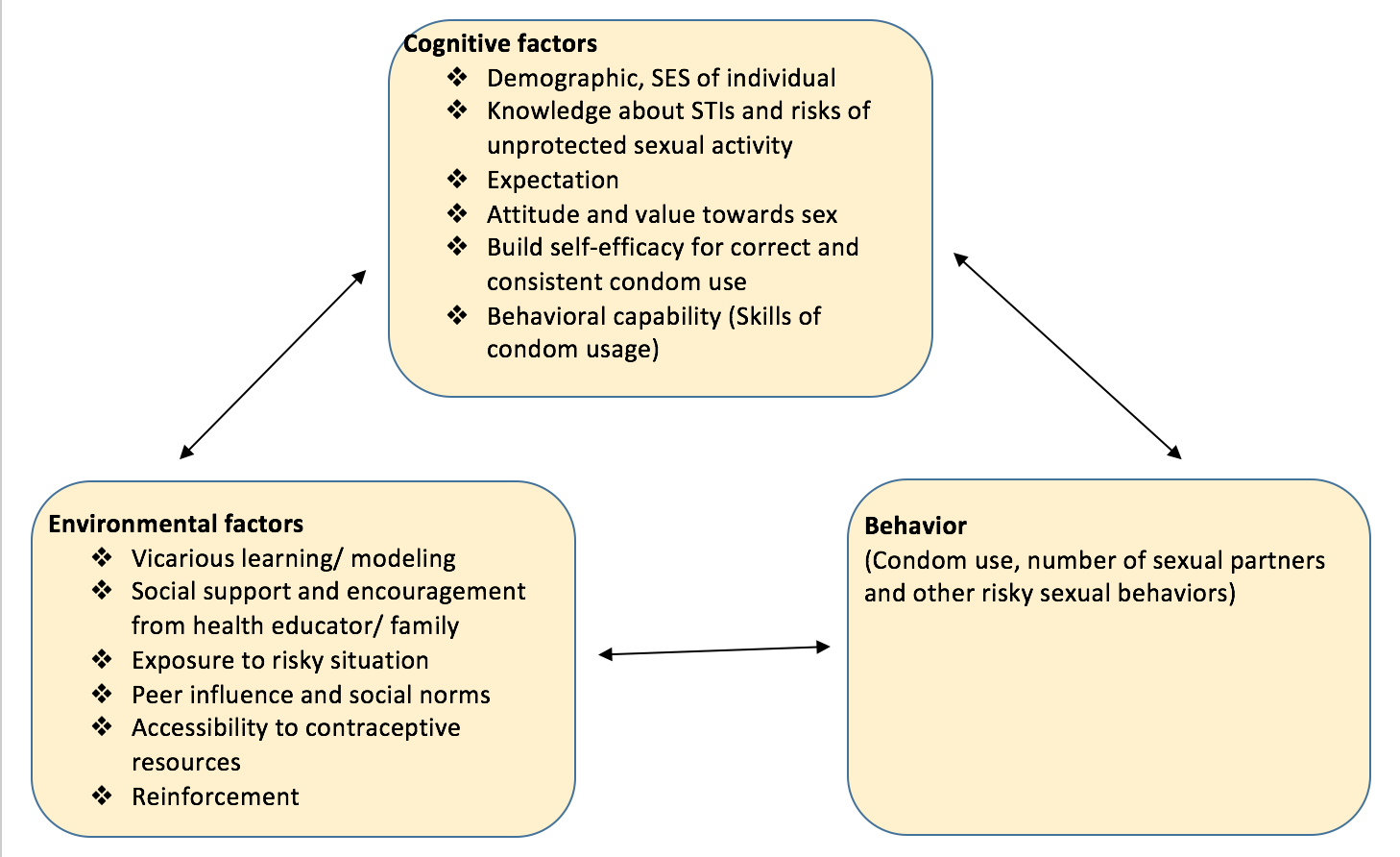
Social Cognitive theory
Social cognitive theory describes a dynamic process in which personal, environmental factors and behaviors influence each other. The social cognitive theory includes 6 constructs: Reciprocal determinism, behavioral capability, expectations, self-efficacy, observational learning, and reinforcement.
Constructs
Reciprocal determinism: Social cognitive model is bidirectional. Each category of the construct in this model determines the other in a feedback loop. There is a dynamic interaction between 1) individual, 2) behavior and 3) environment in the social cognitive theory.Personal factors influence behavior and environment, the environment influence behavior and personal factors. Additionally, behavior affects the environment and personal factors in a feedback loop
Behavioral capability is defined as having knowledge and skills to perform a given behavior. For promoting sexual risk reduction behavior, it is important to promote knowledge about STIs and the negative socioeconomic consequence of unwanted teen pregnancy. A study conducted by Markham, et al. (2012) trained adolescents with condom use skills to increase behavioral capability.
Expectations is defined as the outcomes anticipated from the behavioral change. Indicate the positive outcomes and benefit of practicing safer sexual behaviors (i.e condom use).
Self-efficacy is defined as the confidence in one’s ability to take action. Giving verbal reinforcement, providing training and guidance in sexual risk reduction behavior help to increase self-efficacy of individual is important to encourage adolescents to use condom and other safer sexual behaviors. One study conducted by Donenberg, et al. (2005) measured self-efficacy by asking participants their perception of difficulty using a condom every time. If participants responded ‘Difficult to do’, then it indicates low self-efficacy. On the other hand, if participants responded ‘Very easy to do’ then it indicates high self-efficacy.
Observational learning (modeling) is defined as observing the actions and outcomes of others’ behaviors. In another words, observational learning is learning through other people’s experience, rather than their own experience. By showing negative consequence of risky sexual behaviors like HIV and other STIs, it promotes adolescents to avoid risky sexual behaviors.
Reinforcements is defined as the responses to an individual that increase or decrease reoccurrence of behavior. Motivating adolescents to practice safe sex by positive and negative reinforcement. Positive reinforcement include lower risks for STIs, and negative reinforcement including unwanted pregnancy and risks for HIV and other STIs. Reinforcement is important to motivate adolescents to perform sexual risk reduction behaviors like condom use.
Diagram of Social Cognitive Theory
Part III. Logic Model, Causal and Intervention Hypotheses, and Intervention Strategies
Target population
The intervention program will be targeted for adolescents between the age of 11 to 19 specifically in a minority group or in geographic area with low socioeconomic status, and with a focus on bisexuality and homosexuality.
According to a study conducted by DiClemente, et al (2009) , there is health disparity in STIs and HIV among African American adolescents. Additionally, homosexuality should be another key area of study. According to Wolitski et al (2011), gay and bisexual men are disproportionately affected by STIs compared to heterosexual men in the United States. Adolescents from geographic area with low socioeconomic status are less likely to have access to resources for HIV screening and education about sexual health. Study conducted by Morrison-Beedy et. al (2012) indicated adolescents from low-income urban settings are at elevated risk for unwanted pregnancy, HIV and other STIs.
Intervention setting
Setting for the intervention will take place in a group-based, community setting (i.e. in schools) in a low-socioeconomic status geographic areas with a high population of minorities, specifically African Americans.
Table 2: Intervention Method and strategy
| Intervention Method | Alignment with Theory | Intervention Strategy |
| Learning through observing outcomes of others’ behaviors (Peer role model video) | One of the constructs of the social cognitive theory is observational learning, which is also known as modeling. Observational learning is thought to be important for the learning process of adolescents through experience of credible others. By observing the negative consequence from a behaviors help adolescents to avoid performing risky sexual behaviors. | Show educational videos about people with past experience of risky sexual behaviors and the consequence of risky sexual behaviors. For example, showing existing cases of unplanned pregnancy as a consequence of unprotected sex help adolescents understand the importance of protected sexual activities and the socioeconomic burden of unwanted pregnancy. |
| Provide knowledge about unwanted pregnancy, HIV/STIs, and risks of unprotected sex | Behavioral capability is one of the construct of social cognitive theory. | Promote knowledge about STIs and the negative consequence of unwanted pregnancy, and the risks of unprotected sex through group session, include class activities to help adolescents learn interactively. Condom usage training is also appropriate in this intervention to increase adolescents’ behavioral capability. |
| Develop self-efficacy | One of the constructs of the social cognitive theory is self-efficacy. If adolescents do not have confidence that they can change behavior, it would make behavioral changes difficult. | Giving verbal reinforcement, providing training and guidance in sexual risk reduction behavior. Approach behavioral change in small steps to ensure success and not to overwhelm the adolescents. Let adolescents to reflect what are the specific desired changes and their goals.
|
|
Consider personal, behavioral and environmental factors to promote sexual risk reduction behaviors. Promote positive attitude and values towards sex |
Individual component of social cognitive theory. Reciprocal determinism means that the social cognitive theory is the dynamic interaction of individual, behavioral and environmental factors. These factors exert influence upon each other. Changing attitude is the individual component of the social cognitive theory. If adolescents’ attitudes and values towards sex has changed, this will change the environmental factors and sexual behaviors of adolescents. | Change the attitude and value towards sex and condom use by showing educational videos. Provide social support to motivate adolescents to practice safe sex, which helps to promote positive attitude towards condom use. |
Logic model for group-based risk reduction intervention program
Table 3: Program Logic Model
| Inputs/Resources | Activities | Outputs | Short-term Outcomes | Intermediate Outcomes | Long-term Outcomes |
| -Funding for educational materials (handbooks which includes role play activities, factsheet, videos) are designed and obtained from CDC, training of health educators (selected from teachers from local public school system and healthcare workers from local health clinic or hospital)
-Group based intervention sessions are designed by public health professional from GA state government that has background in health promotion and behaviors. -Funds from government, public health organizations like the Center for Disease Control and prevention. -Partnership with local health clinics and hospitals where healthcare providers can refer participants into the intervention program, and provide sexual health resources -Location of group based session: classrooms in schools that participate in the program
|
Role play training, social support, verbal reinforcement, promote knowledge about STIs, HIV and the negative consequence of unwanted pregnancy through group activities, condom usage training, education about birth control options, show educational videos about people with past experience of risky sexual behaviors and the consequence of risky sexual behaviors. Group discussion about concerns and questions that adolescents may have | 200 Handbooks provided to every participants in the intervention program that includes fact sheets about HIV and STIs, information about contraceptive, location where they can get contraceptive resources. There is also a page for parents to inform them what impact they could make to be socially supportive of adolescents and their verbal reinforcement would help too
10 activities including knowledge about STIs, HIV and the negative consequences of risky sexual behavior, condom usage training activity 20 Educational videos on sexual health # 8 weekly group based sessions 30 health educators will be trained 4 role play training held contact 30 local health clinics and hospitals |
Increase knowledge about STIs, HIV and negative consequences of risky sexual behaviors
-Adolescents are able to identify the negative consequence of risky sexual behaviors and understand the importance of condom usage Increase behavorial capacity Evidence of increase behavioral capability which include 2 components: 1) Evidence of capability of condom usage skills 2) evidence of increased knowledge about HIV, STIs and understand the negative consequence of risky sexual behaviors. Increase self-efficacy Increase adolescent’s self-efficacy, having greater confidence that they are able to make the changes Promote positive attitude and values towards sex
|
Decreases in risky sexual behavior (i.e. Perform protected sex every time, decrease number of sexual partners) | Decrease prevalence of STIs and HIV. Decrease rates of unplanned teen pregnancy. Increase quality of life for adolescents (Decrease incidence of teen pregnancy can prevent the socioeconomic burden of adolescents) |
Intervention hypothesis
-By providing group based sessions on sexual health, educational videos on adolescents health and lectures on STIs and HIV, education about birth control options, this will increase adolescents knowledge about STIs, HIV and negative consequences of risky sexual behaviors and change the attitude and value towards sex.
-By providing condom usage training, providing knowledge on STIs, HIV , this will increase adolescents’ behavioral capacity
-By showing educational videos about people with past experience of risky sexual behaviors and the consequence of risky sexual behaviors, this will promote positive attitude and value towards sex.
By providing verbal reinforcement and social support, it will increase self-efficacy of adolescents.
-Role play training on communications skill with partners will increase behavioral capacity and self-efficacy of adolescents
-By holding group discussion about concerns and questions that adolescents may have, this will increase their behavioral capacity of adolescents as they get an answer from health educator, so that they are more capable of performing safer sexual behavior.
Causal hypothesis
-Increasing behavioral capacity and self-efficacy of adolescents will lead to decrease risky sexual behaviors. -By changing the attitude and values towards sex will decrease risky sexual behaviors, including delay sexual initiation and decrease number of sexual partners.
-By providing knowledge about STIs, HIV and the negative consequence of unwanted pregnancy, it will decrease decrease risky sexual behaviors as adolescents are more aware of the negative consequence of risky sexual behaviors.
-In the long run, increasing self-efficacy, behavioral capacity, changing the attitude and values towards sex, and providing knowledge about STIs, HIV and the negative consequence of unwanted pregnancy will decrease the prevalence of STI, HIV among adolescents, decrease rates of unplanned pregnancy, increase quality of adolescents’ lives and decrease the socioeconomic burden of teen parents.
SMART Objectives
Goal 1: Promote positive attitude and values towards sex
Outcome objective 1: At 3 months follow up, a self reported survey will be given to examine the effects of the intervention program and see if adolescents’ attitude and values towards sex has been changed in a positive way. At least 25% of participants will report an increased positive attitude and values towards sex (e.g. attitude of condom use)
Outcome objective 2: At 6 months follow up, at least 50% of participants report a more positive attitude and values towards sex
Outcome objective 3: At 12 months follow up, at least 75% of participants report an increased positive attitude and values towards sex
Outcome objective 4: At 18 months follow up, the rate of positive attitude and values change towards sex remains the same as 12 months or higher
Goal 2: Increase knowledge about STIs, HIV and negative consequences of risky sexual behaviors
Outcome objective 1: Quiz at the end of each session to see how much information was obtained after attending the session. A cumulative quiz will be given at the last session of the program, to test adolescents knowledge on risky sexual behaviors after participating in the intervention program. 80 is a passing score. 85% of participants will achieve a score of 80 or above.
Goal 3: Increase self-efficacy of adolescents
Outcome objective 1: At 3 months, to measure the self-efficacy of condom use with partners consistently by conducting a self-reported survey. Participants respond ‘easy to do’ (which indicate high self-efficacy) increase by 25% compare to baseline.
Outcome objective 2: At 6 months follow up, at least 50% of participants report ‘easy to do’
Outcome objective 3: At 12 months follow up, at least 75% of participants report ‘easy to do’
Outcome objective 4: At 18 months follow up, the rate of respondents that report ‘easy to do’ remain the same as 12 months (75%).
Goal 4: Increase behavioral capacity
Outcome objective 1: At least 80% of the participants obtain condom use skills from intervention program and is able to demonstrate skills independently (without assistance from health educator) at the end of the intervention program (week 8)
Part IV. Evaluation Design and Measures
Table 4: Stakeholder roles and evaluation questions
| Stakeholder | Role in Intervention | Evaluation Questions from Stakeholder | Effect on Stakeholder of a Successful Program | Effect on Stakeholder of an Unsuccessful Program |
| Adolescents | Participants in the intervention program | What can I benefit from this intervention program?
What are my goals that I hope to achieve from this program?
|
Decrease in risky sexual behaviors
Increase reported condom use Decrease number of sexual partners Increase in knowledge and aware of the negative consequence of risky sexual behaviors Increase self-efficacy and behavioral capacity of adolescents Delay sexual initiation |
No change in condom use
No change in STIs and HIV prevalence No change in prevalence of unwanted teen pregnancy No delay in sexual initiation |
| Parents | Provide social support for adolescents | How will my children be affected by the intervention program?
Will my children become sexually active after participating in the intervention program? |
Help to motivate adolescents in healthy sexual relationship with partners | Do not support public health efforts in sexual educations
Fear to discuss controversial topics with their children (i.e. contraception) |
| Health educators/ Public health workers | help implement program | How can I effectively change the attitude of adolescents on sexual health?
How do we know if the program has a positive impact on adolescents?
|
Able to teach and promote intervention strategies confidently and in an effective way
|
Wasted time and energy invested in the program.
Decrease willingness to help with future programs |
| Government and private public health organization | Provide funding for the program | How much money should be invested in this program?
For how long will the funding continue? Worth it to invest money in this intervention program? |
Increase in willingness to expand the program | Decrease funding for the program
Less resources provided for the program |
Evaluation design: Group randomized control trial
This study will utilize a randomized experimental design with multiple groups, one group will receive the intervention program as treatment; the other group will not receive the intervention program as control. There are pre-test and post-test procedures utilized for both groups.
Scientific notation
R 01 x 02 03 04 05 06 (intervention group)
R 01 02 03 04 05 06 (Control group)
(R=randomization O1= pre-test O2=post test at week 8 (last session of the intervention program) O3=Post-test at 3 months O4=post-test at 6 months O5= post-test at 12 months O6=post-test at 18 months)
Group randomization will be done by randomization of schools, so that there is less chance of contamination among individual participant.
Treatment/intervention group: 8 weeks of group based sexual risk reduction intervention program
Control group: general health promotion topic, no intervention program
Both the treatment group and control group will take pre-test and post-test that measure their attitude and behaviors.
Pre-test at baseline will be taken on the first day of intervention of all groups. Post-tests will be taken at the end of the program at the 8th weeks and at 3, 6, 12,18 months follow up with both control and treatment group. The control group and treatment group will complete tests on the same days and time. The test will test 1) knowledge of HIV/STIs and other risky sexual behaviors 2) attitude, value and intention 3) self-efficacy and behavioral capacity 4) self-reported sexual risky behaviors
Threats to interval validity
Selection: Selection bias is a threat to interval validity. If certain group in the population has a greater likelihood of being included in the study. For example, if more adolescents that already have HIV or STIs are selected to the control group, this will dampen the effects. In order to attenuate this threat, it is important to ensure there is unbiased randomized sampling. Another potential selection bias situation is when people volunteer to be participate into the intervention program. Compared to the non-participants, those that self-participate into the intervention program could be more conscious with sexual health to begin with,which is why they are interested in a program to decrease risky sexual behaviors. In this situation where self-selection occurs, the intervention group are different to the control group at baseline. Again, to minimize the selection bias, it is important to conduct a randomized sampling. This is the reason why this study is designed as an experimental study with randomization.
Attrition: This is a threat to any study design with more than one group. There is differential loss to follow up if more adolescents are censored than the other group. This threat can be minimized if the group based intervention program take place in schools, where the school directory provides all students contact information.
Testing: Since this study has more than one stage (pre- test and post-test), there is potential testing bias. The pre-test may affect the scores on the post-test. Maturation effects such as becoming older and getting educated, people may do better in post-test even without going through the intervention program. With learning effects, participants may become more familiar with the format of the test and the purpose of the experiment. If this is the case, they may be able to develop a strategy to do better in the test. This will create bias and make it more difficult to measure the effects of the intervention program. In order to minimize testing bias, it may be helpful to change the order of the questions in the test.
Recall bias: Recall bias is a type of information bias in a study, which result from inaccurate recall of past exposure. Since some questions like asking participants about number of sexual partners and their past sexual experience are self-reported, it is a threat to interval validity. If participants are not able to recall their past exposure accurately, this will create bias. To minimize these threats, we can encourage adolescents to keep records so that they remember better. Another way to minimize recall bias, is to use some hints or something to help participants to recall memory. Additionally, we can use objective exposure markers like STD lab results or medical record instead of relying on participants’ responses on whether they have history of STDs. Lastly, by asking questions that has a more reasonable timeframe (e.g. ‘Did you have unprotected sex in the past 3 months?’ is easier for adolescents to recall, versus ‘Did you have unprotected sex in the past 4 years?’ is much harder to recall.)
response bias: Since the study is based on self-report, response bias is a threat to interval validity. Participants may under report number of sexual partners, at what age when they are sexually active. Since the topic can be sensitive, adolescents may feel embarrassed to answer the questions, which may cause underreporting on sexual activities. In order to minimize response bias, we can make the survey anonymous so that participants are less worried about judgement and encourage them to be frank.
Table 5: outcome evaluation questions
| Short-term or Intermediate Outcome Variable | Scale, Questionnaire, Assessment Method | Brief Description of Instrument | Example item (for surveys, scales, or questionnaires) | Reliability and/or Validity Description |
| Increase self-efficacy of adolescents | Self-efficacy scale (Zimmerman, et al 2008) was used to measure
1) refusal self-efficacy (confidence of adolescents in ability to say no to their partners) 2) Situational self-efficacy (in certain situation, how confident are they able to negoiate risky situation) 3) condom use self-efficacy (how confident are they to be able to use a condom properly?) |
Likert scale from 1 to 5 where 1 is ‘I strongly believe that I cannot do this’ and 5 is ‘ I definitely can do this’ Zimmerman, et al (2008) | Refusal self-efficacy: ‘How sure are you that you would be able to say no to your partner to have sexual intercourse?’ Zimmerman, et al (2008)
Situational self-efficacy: ”Do you think you are able to tell someone that you didn’t want to go somewhere because of what might happen sexually?’ Zimmerman, et al (2008) Condom self-efficacy: ‘I feel confident that I would remember to use a condom even after I have been drinking’ Zimmerman, et al 2008 |
Cronbach’s alpha for 1) situational self-efficacy scale was 0.81
2) refusal self-efficacy was 0.89 3) Condom self-efficacy was 0.83 (Zimmerman, et al 2008) |
| Increased behavioral capacity | condom ues checklist was used to measure condom use skills by testing adolescents’ knowledge of how to properly use a condom
Stanton, et al 2009 |
The condom use checklist (CUSC) is to measure condom use skills by agreement of responses (whether correct or incorrect) between the checklist and observed skills. There are 17 statements in the condom use checklist. There are 8 steps to using a condom correctly. Answer is either correct or incorrect.
Stanton, et al 2009 |
There are 17 statements in the condom use checklist. There are 8 steps to using a condom correctly. Answer is either correct or incorrect.
‘Tear along one side of the foil, being sure not to rip the condom inside’ ‘Put the condom on anytime before you ejaculate’ Stanton, et al 2009 |
Internal consistency (alpha=0.63)
Stanton, et al 2009 |
| Increased knowledge of STIs, HIV and the negative consequences of risky sexual behaviors. | knowledge of STD transmission, prevention and natural history (Jaworski, et al 2001) | Yes or no answer; 37 item measures was used to assess the knowledge of STD transmission, prevention and natural history (Jaworski, et al 2001) |
‘can you get herpes from a toilet seat?’ (no) ‘It is easy to tell if your partner has STD?’ (no) |
Internal consistency (alpha=0.86)
Jaworski, et al 2001 |
|
Promote positive attitude and values towards sex |
ATCUS, which stands for Attitudes toward condom use scale measures the attitudes towards condom use among adolescents (Masa, et al 2014)
|
ATCUS measure the attitudes towards condom use scale among adolescents. The scale is from 1 to 5; where 1 is disagree a lot and 6 is agree a lot. (Masa, et al 2014) |
‘Do you believe that Condoms are effective in protecting against HIV/AIDS?’ ‘Do you believe that you do not want to use condom because the price of condom is too high to use regularly?’ ‘Do you believe that Condoms reduce sexual pleasure?’ (Masa, et al 2014) |
Internal consistency (alpha= 0.90)
(Jaworski, et al 2001) |
Part V. Process Evaluation and Data Collection Forms
A) Recruitment and enrollment:
School recruitment: Schools will receive letter about the group based intervention program and are asked to fill a school enrollment form
School recruitment letter
Dear __________,
The University of Georgia School of Public Health would like to invite your school to participate in the group based sexual risk reduction intervention program. The goal of this program is to increase self-efficacy, behavioral capacity, knowledge of STIs and HIV and to decrease risky sexual behaviors among adolescents. This intervention program is a 8 weeks intervention program with one session per week, it is intended to target adolescents age 10-19. If you are interested in participating in this intervention program, or have any inquiry, please do not hesitate to contact groupbasedintervention@uga.edu or call 706-_______ for more information.
Sincerely,
Health promotion Group based sexual risk reduction program coordinator
University of Georgia School of Public Health
School enrollment form
| School name | |
| School address | |
| School phone number | |
| School fax number | |
| Number of adolescents that are eligible for the study (age 10-19) |
B) Student recruitment: Parents will receive a letter about the group based intervention program for their children and are asked to fill in a student enrollment form
Student recruitment letter
Dear Parents/Guardian,
In partnership with [school name], we have a group based risk reduction intervention program that targets to adolescents age 10-19. We would like to invite your child to participate in this intervention program. Participants have the opportunity to gain knowledge of STI/HIV and have a better understanding of the negative consequence of risky sexual behavior. This program is a 8 week intervention program in classroom. Sessions will take place after school once a week for 8 weeks. Participants will receive anonymous assessment quizzes in the first, last session of the intervention program. Additionally, we will follow up with the assessment quizzes at 3, 6, 12 and 18 months of the intervention program. This intervention program is free for all students.
If you would like your children to participate in this intervention program, please sign and submit the form to [teacher name]. If you have any inquiry about the intervention program, please do not hesitate to reach out to groupbasedintervention@uga.edu or call 706-_____ for more information
Sincerely,
Health promotion group based sexual risk reduction program coordinator
University of Georgia School of Public Health
Student name: ____________________
Parents/guardian name: _____________
Parents/guardian signature: ___________
Student enrollment form
| Student’s name | |
| Parents/Guardian name | |
| Phone Number | |
| Home address | |
| Agree to participate? | yes/no |
C) Community partners recruitment: to recruit local health clinics and hospitals for partnership, providing resources for participants. Additionally, they are asked to fill in a community partner recruitment form
Community partners recruitment letter
Dear ___,
University of Georgia School of Public Health will have an intervention program and the goal is to decrease risky sexual behaviors among adolescents. This program targets adolescents from age 10-19. We would like to invite you to partner with us. We would be glad to have healthcare professionals to partner with us to provide adolescents in our community intervention to decrease the high prevalence of STIs. If you are interested in being part of the intervention program or have any inquiry about the program, please do not hesitate to call 706-____ or email us at groupbasedintervention@uga.edu
Sincerely,
Health promotion group based sexual risk reduction program coordinator
University of Georgia School of Public Health
Community partner enrollment form
| Organization name | |
| Phone number | |
| Fax number | |
| Address | |
| Agree to partner with UGA school of Public Health? | Yes/No |
Attrition – how will you know if participants complete all of the observations (O’s from your study design) and all of the intervention components (from your Outputs column of your logic model)?In order to know if participants complete all of the observations, there will be an attendance sheet. Students will sign the sheet at the end of each session if they are present for the session.
Attendance sheet
| Student name | Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 | Week 7 | Week 8 |
In order to minimize loss to follow up, students will be asked to fill in basic information like phone number, home address, email, name and date of birth in the first intervention session. This method can maximize follow up
Student Contact information form
| Student’s name | |
| Date of Birth | |
| Telephone number | |
| Home address | |
| Parent/ Legal Guardian Name |
Assessment test completion: there is one pretest and posttest at week 8 and 3, 6,12, 18 months follow up post test for all participants. In order to keep track of which assessment test was completed by participants, there is a form to keep record. Each student will be given a unique ID, so that we can keep the assessment test as anonymous. (01=pretest at week 1; 02=posttest at week 8; 03=posttest at 3 months; 04=posttest at 6 months; 05= posttest at 12 months; 06=posttest at 18 months)
Assessment test completion form
| Unique ID | o1 | 02 | 03 | 04 | 05 | 06 |
Fidelity of the program – how will you know if the intervention was implemented as you had planned? This should match your Outputs column of your logic model.
| Criteria | 100%-75% | 50-74% | 25%-49% | 0%-24% | Any barriers/obstacles to complete criteria | If any, please provide explanation |
| Handbook and learning material distributed to students in the intervention program? | ||||||
| Were all 2o educational videos presented on appropriate sessions? | ||||||
| Were group activities conducted on appropriate sessions? | ||||||
| Were role play training conducted on appropriate sessions? | ||||||
| Were students engaging in class? | ||||||
| Were all 8 sessions completed over 8 weeks? | ||||||
| How many sessions were completed over 8 weeks? |
Reference
DiClemente, R.J., Wingood, G.M., Rose, E.S., Sales, J.M., Lang, D.L., Caliendo, A.M., Hardin, J.W., Crosby, R.A. (2009). Efficacy of Sexually Transmitted Disease/ Human Immunodeficiency Virus Sexual Risk-Reduction Intervention for African American Adolescent Females Seeking Sexual Health Services: A Randomized Controlled Trial. Archives of Pediatrics and Adolescent Medicine Journal, 163(12):1112-21.
Donenberg, G.R., Pao, M. (2005). Youths and HIV/AIDS: Psychiatry’s Role in a Changing Epidemic. Journal of the American Academy of Child and Adolescent Psychiatry, 44(8):728-47.
Jaworski, B. C., Carey, M. P. Effects of a Brief, Theory-Based STD- Prevention Program for Female College Students. Journal of Adolescent Health. 29(6): 417-425.
Markham, C. M., Tortolero, S. R., Peskin, M.F., Shegog, R., Thiel, M., Baumler, E.R., Addy, R.C. , Escobar-Chaves, S.L., Reininger, B., Robin, L. (2012). Sexual Risk Avoidance and Sexual Risk Reduction Interventions For Middleschool Youth: A Randomized Controlled trial. Journal of Adolescent Health, 50(3):279-88.
Masa, R.D., Chowa, G.A. (2014). HIV Risk Among Young Ghanaians in High School: Validation of a multidimensional Attitude Towards Condom Use Scale. International Journal of Adolescence and Youth, 19(4):444-457.
Morrison-Beedy, D., Jones, S.H., Xia, Y., Tu, X., Crean, H.F., Carey, M.P. (2013). Reducing Sexual Risk Behavior in Adolescent Girls: Results from a Randomized Controlled Trial. Journal of Adolescent Health, 52(3):314-21.
Stanton, B., Deveaux, L., Lunn, S., Yu, S., Brathwaite, N., Li, X., Cottrell, L., Harris, C., Clemens, R., Marshall, S. (2009). Condom-Use Skills Checklist: A Proxy for Assessing Condom-Use Knowledge and Skills When Direct Observation is Not Possible. Journal of Health, Population and Nutrition, 27(3):406-13.
Wolitski, R. J., Fenton. K.A. (2011). Sexual Health, HIV, and Sexually Transmitted Infections among Gay, Bisexual, and Other Men Who Have Sex with Men in the United States. AIDS and Behaviors, 15 Suppl 1:S9-17.
Zimmerman, R.S., Cupp, P.K., Donohew, L., Sionéan, C.K., Feist-Price, S., Helme, D. (2008). Effects of a School-Based, Theory-Driven HIV and Pregnancy Prevention Curriculum. Perspectives on Sexual and Reproductive Health, 40(1):42-51.
